O. Reg. 403/96: STATUTORY ACCIDENT BENEFITS SCHEDULE - ACCIDENTS ON OR AFTER NOVEMBER 1, 1996, Insurance Act, R.S.O. 1990, c. I.8
Insurance Act
ONTARIO REGULATION 403/96
Amended to O. Reg. 314/05
STATUTORY ACCIDENT BENEFITS SCHEDULE — ACCIDENTS ON OR AFTER NOVEMBER 1, 1996
Historical version for the period June 13, 2005 to October 27, 2005.
This is the English version of a bilingual regulation.
CONTENTS
|
|
|
Sections |
|
GENERAL |
|
|
|
|
1 |
|
|
|
2 |
|
|
|
3 |
|
|
INCOME REPLACEMENT BENEFIT |
|
|
|
|
4 |
|
|
|
5 |
|
|
|
6 |
|
|
|
Collateral Payments for Loss of Income and Maximum Amount of Benefit |
7 |
|
|
8 |
|
|
|
9 |
|
|
|
10 |
|
|
|
11 |
|
|
NON-EARNER BENEFIT |
12 |
|
|
CAREGIVER BENEFIT |
13 |
|
|
MEDICAL, REHABILITATION AND ATTENDANT CARE BENEFITS |
|
|
|
|
14 |
|
|
|
15 |
|
|
|
16 |
|
|
|
17 |
|
|
|
Duration of Medical, Rehabilitation and Attendant Care Benefits |
18 |
|
|
Maximum Limits on Medical, Rehabilitation and Attendant Care Benefits |
19 |
|
PAYMENT OF OTHER EXPENSES |
|
|
|
|
20 |
|
|
|
21 |
|
|
|
22 |
|
|
|
23 |
|
|
|
24 |
|
|
DEATH AND FUNERAL BENEFITS |
|
|
|
|
25 |
|
|
|
26 |
|
|
OPTIONAL BENEFITS |
|
|
|
|
27 |
|
|
|
28 |
|
|
|
29 |
|
|
GENERAL EXCLUSIONS |
30 |
|
|
PROCEDURES FOR CLAIMING BENEFITS |
|
|
|
|
31 |
|
|
|
32 |
|
|
|
33 |
|
|
|
34 |
|
|
|
Payment of Income Replacement, Non-earner or Caregiver Benefit |
35 |
|
|
Election of Income Replacement, Non-earner or Caregiver Benefit |
36 |
|
|
Refusal or Stoppage of Income Replacement, Non-earner or Caregiver Benefit |
37 |
|
|
37.1-37.2 |
|
|
|
38-38.1 |
|
|
|
38.2 |
|
|
|
38.3 |
|
|
|
39 |
|
|
|
40 |
|
|
|
41 |
|
|
|
42 |
|
|
|
43 |
|
|
|
44 |
|
|
|
45 |
|
|
|
46 |
|
|
|
47 |
|
|
|
48 |
|
|
|
49 |
|
|
|
50 |
|
|
|
51 |
|
|
DESIGNATED ASSESSMENT CENTRES |
|
|
|
|
52-52.2 |
|
|
|
53-54 |
|
|
RESPONSIBILITY TO OBTAIN TREATMENT, PARTICIPATE IN REHABILITATION AND SEEK EMPLOYMENT |
|
|
|
|
55 |
|
|
|
56 |
|
|
INTERACTION WITH OTHER SYSTEMS |
|
|
|
|
57 |
|
|
|
58 |
|
|
|
59 |
|
|
|
60 |
|
|
INCOME CALCULATION |
|
|
|
|
61 |
|
|
|
62 |
|
|
|
63 |
|
|
|
64 |
|
|
|
64.1 |
|
|
MISCELLANEOUS |
|
|
|
|
65 |
|
|
|
66 |
|
|
|
67 |
|
|
|
68 |
|
|
|
69 |
|
|
|
70-71 |
|
|
Assessment of attendant care needs |
|
1. This Regulation may be cited as the Statutory Accident Benefits Schedule — Accidents on or after November 1, 1996. O. Reg. 462/96, s. 2.
Definitions and Interpretation
2. (1) In this Regulation,
“accident” means an incident in which the use or operation of an automobile directly causes an impairment or directly causes damage to any prescription eyewear, denture, hearing aid, prosthesis or other medical or dental device; (“accident”)
“attendant care benefit” means the benefit provided by section 16; (“indemnité de soins auxiliaires”)
“business day” means a day that is not,
(a) Saturday, or
(b) a holiday within the meaning of subsection 29 (1) of the Interpretation Act, other than Easter Monday and Remembrance Day; (“jour ouvrable”)
“caregiver benefit” means the benefit provided by Part IV; (“indemnité de soignant”)
“case manager” means a person who provides services related to the coordination of goods or services for which payment is provided by a medical, rehabilitation or attendant care benefit; (“gestionnaire de cas”)
“chiropractor” means a person authorized by law to practise chiropractic; (“chiropraticien”)
“death benefit” means the benefit provided by section 25; (“prestation de décès”)
“dentist” means a person authorized by law to practise dentistry; (“dentiste”)
“designated assessment” means an assessment arranged or conducted by a designated assessment centre under section 43; (“évaluation désignée”)
“designated assessment centre” means an assessment centre designated under section 52; (“centre d’évaluation désigné”)
“funeral benefit” means the benefit provided by section 26; (“indemnité pour frais funéraires”)
“Grade I Whiplash Guideline” means the Pre-approved Framework Guideline entitled Pre-approved Framework Guideline for Whiplash Associated Disorder Grade I Injuries With or Without Complaint of Back Symptoms; (“lignes directrices pour les entorses cervicales de stade I”)
“Grade II Whiplash Guideline” means the Pre-approved Framework Guideline entitled Pre-approved Framework Guideline for Whiplash Associated Disorder Grade II Injuries With or Without Complaint of Back Symptoms; (“lignes directrices pour les entorses cervicales de stade II”)
“Guideline” means,
(a) a guideline issued by the Superintendent under subsection 268.3 (1) of the Act that is published in The Ontario Gazette,
(b) a Pre-approved Framework Guideline,
(c) a guideline that is included in the professional fee guidelines, the Transportation Expense Guidelines or the Optional Indexation Benefit Guidelines, as published in The Ontario Gazette by the Ontario Insurance Commission or Financial Services Commission of Ontario,
(d) a guideline published in The Ontario Gazette that is an amended version of a guideline referred to in clause (a), (b) or (c); (“directive”)
“health practitioner”, in respect of a particular impairment, means a physician or,
(a) a chiropractor, if the impairment is one that a chiropractor is authorized by law to treat,
(b) a dentist, if the impairment is one that a dentist is authorized by law to treat,
(b.1) an occupational therapist, if the impairment is one that an occupational therapist is authorized by law to treat,
(c) an optometrist, if the impairment is one that an optometrist is authorized by law to treat,
(d) a psychologist, if the impairment is one that a psychologist is authorized by law to treat,
(e) a physiotherapist, if the impairment is one that a physiotherapist is authorized by law to treat; (“praticien de la santé”)
(f) a registered nurse with an extended certificate of registration, if the impairment is one that the nurse is authorized by law to treat, or
(g) a speech-language pathologist, if the impairment is one that a speech-language pathologist is authorized by law to treat;
“impairment” means a loss or abnormality of a psychological, physiological or anatomical structure or function; (“déficience”)
“income replacement benefit” means the benefit provided by Part II; (“indemnité de remplacement de revenu”)
“insured automobile”, in respect of a particular motor vehicle liability policy, means any automobile covered by the policy; (“automobile assurée”)
“insured person”, in respect of a particular motor vehicle liability policy, means,
(a) the named insured, any person specified in the policy as a driver of the insured automobile, the spouse of the named insured and any dependant of the named insured or spouse, if the named insured, specified driver, spouse or dependant,
(i) is involved in an accident in or outside Ontario that involves the insured automobile or another automobile, or
(ii) is not involved in an accident but suffers psychological or mental injury as a result of an accident in or outside Ontario that results in a physical injury to his or her spouse, child, grandchild, parent, grandparent, brother, sister, dependant or spouse’s dependant,
(b) in respect of accidents in Ontario, a person who is involved in an accident involving the insured automobile, and
(c) in respect of accidents outside Ontario, a person who is an occupant of the insured automobile and who is a resident of Ontario or was a resident of Ontario at some point during the 60 days before the accident; (“personne assurée”)
“medical benefit” means the benefit provided by section 14; (“indemnité pour frais médicaux”)
“member of a health profession” means a member of a College as defined in the Regulated Health Professions Act, 1991; (“membre d’une profession de la santé”)
“non-earner benefit” means the benefit provided by Part III; (“indemnité de personne sans revenu d’emploi”)
“occupational therapist” means a person authorized by law to practise occupational therapy; (“ergothérapeute”)
“optometrist” means a person who is authorized by law to practise optometry; (“optométriste”)
“person in need of care” means, in respect of an insured person, another person who is less than 16 years of age or who requires care because of physical or mental incapacity; (“personne ayant besoin de soins”)
“personal and vocational characteristics” include,
(a) employment history,
(b) education and training,
(c) vocational aptitudes,
(d) vocational skills,
(e) physical abilities,
(f) cognitive abilities, and
(g) language abilities; (“caractéristiques personnelles et professionnelles”)
“physician” means a person authorized by law to practise medicine; (“médecin”)
“Pre-approved Framework Guideline” means a guideline,
(a) that is issued by the Superintendent under subsection 268.3 (1.1) of the Act and published in The Ontario Gazette, and
(b) which establishes, in respect of one or more impairments, a treatment framework; (“directive relative à un cadre de traitement préapprouvé”)
“psychologist” means a person authorized by law to practise psychology; (“psychologue”)
“physiotherapist” means a person authorized by law to practice physiotherapy; (“physiothérapeute”)
“registered nurse with an extended certificate of registration” means a person authorized by law to practise nursing who holds an extended certificate of registration under the Nursing Act, 1991; (“infirmière autorisée ou infirmier autorisé titulaire d’un certificat d’inscription supérieur”)
“rehabilitation benefit” means the benefit provided by section 15; (“indemnité de réadaptation”)
“speech-language pathologist” means a person authorized by law to practise speech-language pathology; (“orthophoniste”)
“spouse” has the same meaning as in Part VI of the Insurance Act; (“conjoint”) O. Reg. 403/96, s. 2 (1); O. Reg. 114/00, s. 1 (1, 2); O. Reg. 281/03, s. 1 (1-4); O. Reg. 458/03, s. 1; O. Reg. 314/05, s. 1 (1, 2).
(1.1) For the purposes of this Regulation, a catastrophic impairment caused by an accident that occurs before October 1, 2003 is,
(a) paraplegia or quadriplegia;
(b) the amputation or other impairment causing the total and permanent loss of use of both arms;
(c) the amputation or other impairment causing the total and permanent loss of use of both an arm and a leg;
(d) the total loss of vision in both eyes;
(e) brain impairment that, in respect of an accident, results in,
(i) a score of 9 or less on the Glasgow Coma Scale, as published in Jennett, B. and Teasdale, G., Management of Head Injuries, Contemporary Neurology Series, Volume 20, F.A. Davis Company, Philadelphia, 1981, according to a test administered within a reasonable period of time after the accident by a person trained for that purpose, or
(ii) a score of 2 (vegetative) or 3 (severe disability) on the Glasgow Outcome Scale, as published in Jennett, B. and Bond, M., Assessment of Outcome After Severe Brain Damage, Lancet i:480, 1975, according to a test administered more than six months after the accident by a person trained for that purpose;
(f) subject to subsections (2) and (3), an impairment or combination of impairments that, in accordance with the American Medical Association’s Guides to the Evaluation of Permanent Impairment, 4th edition, 1993, results in 55 per cent or more impairment of the whole person; or
(g) subject to subsections (2) and (3), an impairment that, in accordance with the American Medical Association’s Guides to the Evaluation of Permanent Impairment, 4th edition, 1993, results in a class 4 impairment (marked impairment) or class 5 impairment (extreme impairment) due to mental or behavioural disorder. O. Reg. 281/03, s. 1 (5); O. Reg. 314/05, s. 1 (1, 2).
(1.2) For the purposes of this Regulation, a catastrophic impairment caused by an accident that occurs after September 30, 2003 is,
(a) paraplegia or quadriplegia;
(b) the amputation or other impairment causing the total and permanent loss of use of both arms or both legs;
(c) the amputation or other impairment causing the total and permanent loss of use of one or both arms and one or both legs;
(d) the total loss of vision in both eyes;
(e) subject to subsection (1.4), brain impairment that, in respect of an accident, results in,
(i) a score of 9 or less on the Glasgow Coma Scale, as published in Jennett, B. and Teasdale, G., Management of Head Injuries, Contemporary Neurology Series, Volume 20, F.A. Davis Company, Philadelphia, 1981, according to a test administered within a reasonable period of time after the accident by a person trained for that purpose, or
(ii) a score of 2 (vegetative) or 3 (severe disability) on the Glasgow Outcome Scale, as published in Jennett, B. and Bond, M., Assessment of Outcome After Severe Brain Damage, Lancet i:480, 1975, according to a test administered more than six months after the accident by a person trained for that purpose;
(f) subject to subsections (1.4), (2.1) and (3), an impairment or combination of impairments that, in accordance with the American Medical Association’s Guides to the Evaluation of Permanent Impairment, 4th edition, 1993, results in 55 per cent or more impairment of the whole person; or
(g) subject to subsections (1.4), (2.1) and (3), an impairment that, in accordance with the American Medical Association’s Guides to the Evaluation of Permanent Impairment, 4th edition, 1993, results in a class 4 impairment (marked impairment) or class 5 impairment (extreme impairment) due to mental or behavioural disorder. O. Reg. 281/03, s. 1 (5).
(1.3) Subsection (1.4) applies if an insured person is under the age of 16 years at the time of the accident and none of the Glasgow Coma Scale, the Glasgow Outcome Scale or the American Medical Association’s Guides to the Evaluation of Permanent Impairment, 4th edition, 1993, referred to in clause (1.2) (e), (f) or (g) can be applied by reason of the age of the insured person. O. Reg. 281/03, s. 1 (5).
(1.4) For the purposes of clauses (1.2) (e), (f) and (g), an impairment sustained in an accident by an insured person described in subsection (1.3) that can reasonably be believed to be a catastrophic impairment shall be deemed to be the impairment that is most analogous to the impairment referred to in clause (1.2) (e), (f) or (g), after taking into consideration the developmental implications of the impairment. O. Reg. 281/03, s. 1 (5).
(2) Clauses (1.1) (f) and (g) do not apply in respect of an insured person who sustains an impairment as a result of an accident that occurs before October 1, 2003 unless,
(a) the insured person’s health practitioner states in writing that the insured person’s condition has stabilized and is not likely to improve with treatment; or
(b) three years have elapsed since the accident. O. Reg. 403/96, s. 2 (2); O. Reg. 281/03, s. 1 (6).
(2.1) Clauses (1.2) (f) and (g) do not apply in respect of an insured person who sustains an impairment as a result of an accident that occurs after September 30, 2003 unless,
(a) the insured person’s health practitioner states in writing that the insured person’s condition is unlikely to cease to be a catastrophic impairment; or
(b) two years have elapsed since the accident. O. Reg. 281/03, s. 1 (7).
(3) For the purpose of clauses (1.1) (f) and (g) and (1.2) (f) and (g), an impairment that is sustained by an insured person but is not listed in the American Medical Association’s Guides to the Evaluation of Permanent Impairment, 4th edition, 1993 shall be deemed to be the impairment that is listed in that document and that is most analogous to the impairment sustained by the insured person. O. Reg. 403/96, s. 2 (3); O. Reg. 281/03, s. 1 (8).
(4) For the purpose of this Regulation, a person suffers a complete inability to carry on a normal life as a result of an accident if, and only if, as a result of the accident, the person sustains an impairment that continuously prevents the person from engaging in substantially all of the activities in which the person ordinarily engaged before the accident. O. Reg. 403/96, s. 2 (4).
(5) For the purpose of this Regulation, a person is employed if, for salary, wages, other remuneration or profit, the person is engaged in employment, including self-employment, or is the holder of an office, and “employment” has a corresponding meaning. O. Reg. 403/96, s. 2 (5).
(6) For the purpose of this Regulation, a person is a dependant of another person if the person is principally dependent for financial support or care on the other person or the other person’s spouse. O. Reg. 403/96, s. 2 (6); O. Reg. 114/00, s. 1 (3); O. Reg. 314/05, s. 1 (3).
(7) For the purpose of this Regulation, an aide or attendant for a person includes a family member or friend who acts as the person’s aide or attendant, even if the family member or friend does not possess any special qualifications. O. Reg. 403/96, s. 2 (7).
(8) For the purpose of this Regulation, payments of severance pay or termination pay are not payments for loss of income. O. Reg. 403/96, s. 2 (8).
(9) For the purpose of this Regulation, payments for loss of income under an income continuation benefit plan shall be deemed to include the following payments:
1. Payments of disability pension benefits under the Canada Pension Plan.
2. Periodic payments of insurance, if the insurance,
i. is offered by the insurer only to persons who are employed at the time the contract for the insurance is entered into, and
ii. is offered by the insurer only on the basis that the maximum benefit payable is limited to an amount calculated with reference to the insured person’s income from employment. O. Reg. 482/01, s. 1.
(10) Subsection (9) only applies in respect of accidents that occur on or after January 1, 2002. O. Reg. 482/01, s. 1.
3. (1) The benefits set out in this Regulation shall be provided under every contract evidenced by a motor vehicle liability policy in respect of accidents occurring on or after November 1, 1996. O. Reg. 403/96, s. 3 (1); O. Reg. 462/96, s. 3.
(2) The benefits set out in this Regulation shall be provided in respect of accidents that occur in Canada or the United States of America, or on a vessel plying between ports of Canada or the United States of America.
(3) Benefits payable under this Regulation in respect of an insured person shall be paid by the insurer that is liable to pay under subsection 268 (2) of the Insurance Act.
(4) Subject to Part IX, the insurer shall pay the benefits under this Regulation despite section 225, subsection 233 (1), section 240 and subsection 265 (3) of the Insurance Act. O. Reg. 403/96, s. 3 (2-4).
PART II
INCOME REPLACEMENT BENEFIT
4. (1) The insurer shall pay an insured person who sustains an impairment as a result of an accident an income replacement benefit if the insured person meets any of the following qualifications:
1. The insured person was employed at the time of the accident and, as a result of and within 104 weeks after the accident, suffers a substantial inability to perform the essential tasks of that employment.
2. The insured person,
i. was not employed at the time of the accident,
ii. was employed for at least 26 weeks during the 52 weeks before the accident or was receiving benefits under the Employment Insurance Act (Canada) at the time of the accident,
iii. was 16 years of age or more or was excused from attendance at school under the Education Act at the time of the accident, and
iv. as a result of and within 104 weeks after the accident, suffers a substantial inability to perform the essential tasks of the employment in which the insured person spent the most time during the 52 weeks before the accident.
3. The insured person,
i. was entitled at the time of the accident to start work within one year under a legitimate contract of employment that was made before the accident and that is evidenced in writing, and
ii. as a result of and within 104 weeks after the accident, suffers a substantial inability to perform the essential tasks of the employment he or she was entitled to start under the contract. O. Reg. 403/96, s. 4.
(2) Despite subsection (1), paragraph 3 of that subsection applies only if the accident occurs before April 15, 2004. O. Reg. 458/03, s. 2.
5. (1) Subject to subsection (2), an income replacement benefit is payable during the period that the insured person suffers a substantial inability to perform the essential tasks of the employment in respect of which he or she qualifies for the benefit under section 4. O. Reg. 403/96, s. 5 (1).
(2) The insurer is not required to pay an income replacement benefit,
(a) for the first week of the disability;
(b) for any period longer than 104 weeks of disability, unless, as a result of the accident, the insured person is suffering a complete inability to engage in any employment for which he or she is reasonably suited by education, training or experience;
(c) in the case of an insured person who qualifies for the benefit under paragraph 3 of section 4, for the period before the day he or she would have been entitled under the contract to begin employment;
(d) for any period longer than 12 weeks after the accident, in the case of an insured person whose impairment comes within the Grade I Whiplash Guideline, if the accident occurred after April 14, 2004; or
(e) for any period longer than 16 weeks after the accident, in the case of an insured person whose impairment comes within the Grade II Whiplash Guideline, if the accident occurred after April 14, 2004. O. Reg. 403/96, s. 5 (2); O. Reg. 458/03, s. 3.
6. (1) The amount of the income replacement benefit shall be,
(a) for each of the first 104 weeks of disability, 80 per cent of the insured person’s net weekly income from employment determined in accordance with section 61; and
(b) for each week after the first 104 weeks of disability, the greater of the amount specified in clause (a) and $185.
(2) The insurer may deduct from the amount of the income replacement benefit payable to an insured person 80 per cent of the net income received by the insured person in respect of any employment subsequent to the accident.
(3) For the purpose of subsection (2), the net income received by an insured person in respect of employment subsequent to the accident shall be determined by subtracting the following amounts from the gross income received by the person in respect of the employment subsequent to the accident:
1. The premium payable by the person under the Employment Insurance Act (Canada) on the gross income.
2. The contribution payable by the person under the Canada Pension Plan on the gross income.
3. The income tax payable by the person under the Income Tax Act (Canada) and the Income Tax Act (Ontario) on the gross income.
(4) For the purpose of subsection (2), net income from self-employment for an insured person who was self-employed at the time of the accident shall be determined without making any deductions for,
(a) expenses that were not reasonable or necessary to prevent a loss of revenue;
(b) salary expenses that were paid to replace the person’s active participation in the business, except to the extent that those expenses were reasonable for that purpose; and
(c) non-salary expenses that were different in nature or greater than the non-salary expenses incurred before the accident, except to the extent that those expenses were necessary to prevent or reduce any losses resulting from the accident.
(5) If the insured person was self-employed at the time of the accident and the person incurs losses from self-employment as a result of the accident, the insurer shall add to the amount of the income replacement benefit payable to the person 80 per cent of the losses from self-employment incurred as a result of the accident.
(6) For the purpose of subsection (5), losses from self-employment shall be determined in the same manner as losses from the business in which the person was self-employed would be determined under subsection 9 (2) of the Income Tax Act (Canada) and the Income Tax Act (Ontario), without making any deductions for,
(a) expenses that were not reasonable or necessary to prevent a loss of revenue;
(b) salary expenses that were paid to replace the person’s active participation in the business, except to the extent that those expenses were reasonable for that purpose;
(c) non-salary expenses that were different in nature or greater than the non-salary expenses incurred before the accident, except to the extent that those expenses were necessary to prevent or reduce any losses resulting from the accident;
(d) expenses that are eligible for capital cost allowance or an allowance on eligible capital property; or
(e) losses deductible under section 111 of the Income Tax Act (Canada). O. Reg. 403/96, s. 6.
Collateral Payments for Loss of Income and Maximum Amount of Benefit
7. (1) Despite subsections 6 (1) and (5), but subject to subsection 6 (2), the weekly amount of an income replacement benefit payable to a person shall be the lesser of the following amounts:
1. The amount determined under subsections 6 (1) and (5), reduced by,
i. net weekly payments for loss of income that are being received by the person as a result of the accident under the laws of any jurisdiction or under any income continuation benefit plan, and
ii. net weekly payments for loss of income that are not being received by the person but are available to the person as a result of the accident under the laws of any jurisdiction or under any income continuation benefit plan, unless the person has applied to receive the payments for loss of income.
2. The greater of the following amounts:
i. $400.
ii. If the optional income replacement benefit referred to in section 27 has been purchased and is applicable to the person, the amount fixed by the optional benefit. O. Reg. 403/96, s. 7 (1); O. Reg. 462/96, s. 4; O. Reg. 281/03, s. 2 (1, 2).
(2) For the purposes of paragraph 1 of subsection (1), the amount determined under subsections 6 (1) and (5) shall not be reduced by,
(a) benefits under the Employment Insurance Act (Canada) that are being received by or are available to the person;
(b) payments under a sick leave plan that are not being received by the person but are available to the person; or
(c) payments under a workers’ compensation law or plan that are not being received by the person and to which the person is not entitled because the person has elected under the workers’ compensation law or plan to bring an action. O. Reg. 403/96, s. 7 (2); O. Reg. 281/03, s. 2 (3).
(3) For the purpose of this section, net weekly payments for loss of income shall be determined by subtracting from the gross weekly amount of payments for loss of income the income tax payable by the person under the Income Tax Act (Canada) and the Income Tax Act (Ontario) on the gross weekly amount of payments for loss of income. O. Reg. 403/96, s. 7 (3).
(4) For the purpose of subsection (3), the person whose net weekly payments for loss of income are to be determined shall be deemed to be a resident of Ontario. O. Reg. 403/96, s. 7 (4).
8. (1) An insured person who is eligible for an income replacement benefit under paragraph 1 of section 4 and who was not self-employed at any time during the four weeks before the accident shall designate one of the following time periods:
1. The four weeks before the accident.
2. The 52 weeks before the accident.
(2) An insured person who is eligible for an income replacement benefit under paragraph 1 of section 4 and who was self-employed at any time during the four weeks before the accident shall designate one of the following time periods:
1. The 52 weeks before the accident.
2. The last fiscal year completed before the accident for the business in which the person was self-employed, if the business completed a fiscal year before the accident. O. Reg. 403/96, s. 8 (1, 2).
(3) For the purpose of determining the amount of an insured person’s income replacement benefit, the gross annual income from employment for a person who qualifies for a benefit under paragraph 1 of section 4 shall be deemed to be the following amount:
1. In the case of a person who designated the four weeks before the accident under paragraph 1 of subsection (1), the person’s gross income from employment for the four weeks before the accident, multiplied by 13.
2. In the case of a person who designated the 52 weeks before the accident under paragraph 2 of subsection (1) or paragraph 1 of subsection (2), the person’s gross income from employment for the 52 weeks before the accident.
3. In the case of a person who designated the last fiscal year completed before the accident under paragraph 2 of subsection (2), the person’s gross income from employment for that fiscal year. O. Reg. 403/96, s. 8 (3); O. Reg. 462/96, s. 5.
(4) For the purpose of determining the amount of an insured person’s income replacement benefit, the gross annual income from employment for a person who qualifies for a benefit under paragraph 2 of section 4 shall be deemed to be the person’s gross income from employment for the 52 weeks before the accident.
(5) For the purpose of determining the amount of an insured person’s income replacement benefit, the gross annual income from employment for a person who qualifies for a benefit under paragraph 3 of section 4 shall be deemed to be the gross income payable under the contract of employment, extrapolated to reflect an annual income.
(6) A determination of gross income under subsection (3) or (4) shall include any benefits received under the Employment Insurance Act (Canada) or a predecessor of that Act in respect of the relevant period.
(7) If a person qualifies for an income replacement benefit under paragraph 1 or 2 of section 4 and also qualifies under paragraph 3 of section 4, the person’s gross annual income from employment shall be determined under subsection (3) or (4), as the case may be, until the day he or she would have been entitled to begin employment under the contract described in paragraph 3 of section 4, and thereafter the person’s gross annual income from employment shall be determined in accordance with subsection (5). O. Reg. 403/96, s. 8 (4-7).
9. (1) Despite sections 6 and 7, if a person is receiving an income replacement benefit immediately before attaining 65 years of age, the weekly amount of the benefit shall be adjusted, on the later of the date the person attains 65 years of age and the second anniversary of the date the person began receiving the benefit, to the amount determined in accordance with the following formula:
![]()
where,
A = the amount to which the weekly amount of the income replacement benefit shall be adjusted,
B = the weekly amount of the income replacement benefit that the person was entitled to receive immediately before the adjustment, including any additions required by subsection 6 (5) but without making any deductions permitted by subsection 6 (2),
C = the lesser of,
i. 35, and
ii. the number of years during which the person qualified for the income replacement benefit before the adjustment is made.
(2) An income replacement benefit that has been adjusted under subsection (1) is payable until the person dies.
(3) Section 5 and subsections 6 (2) to (6) do not apply to an income replacement benefit that has been adjusted under subsection (1). O. Reg. 403/96, s. 9.
Entitlement Arising after Age 65
10. (1) Despite sections 6 and 7, if a person becomes entitled to receive an income replacement benefit after attaining 65 years of age, the weekly amount of the benefit shall be the amount determined under section 7 multiplied by the factor set out in Column 2 of the Table to this subsection opposite the number of weeks that have elapsed since the person became entitled to receive the benefit.
TABLE
|
Column 1 |
Column 2 |
|
Number of weeks since Entitlement Arose |
Factor |
|
Less than 52 weeks |
1.0 |
|
52 weeks or more but less than 104 weeks |
0.8 |
|
104 weeks or more but less than 156 weeks |
0.6 |
|
156 weeks or more but less than 208 weeks |
0.3 |
|
208 weeks or more |
0.0 |
(2) An income replacement benefit is no longer payable to a person to whom subsection (1) applies if more than 208 weeks have elapsed since the person became entitled to the benefit.
(3) Subsections 6 (2) to (6) do not apply to the income replacement benefit paid to a person to whom subsection (1) applies. O. Reg. 403/96, s. 10.
Temporary Return to Employment
11. A person receiving an income replacement benefit may return to or start an employment at any time during the 104 weeks following the onset of the disability in respect of which the benefit is paid without affecting his or her entitlement to resume receiving benefits under this Part if, as a result of the accident, he or she is unable to continue in the employment. O. Reg. 403/96, s. 11.
12. (1) The insurer shall pay an insured person who sustains an impairment as a result of an accident a non-earner benefit if the insured person meets any of the following qualifications:
1. The insured person suffers a complete inability to carry on a normal life as a result of and within 104 weeks after the accident and does not qualify for an income replacement benefit.
2. The insured person suffers a complete inability to carry on a normal life as a result of and within 104 weeks after the accident, received a caregiver benefit as a result of the accident and there is no longer a person in need of care.
3. The insured person suffers a complete inability to carry on a normal life as a result of and within 104 weeks after the accident and,
i. was enrolled on a full-time basis in elementary, secondary or post-secondary education at the time of the accident, or
ii. completed his or her education less than one year before the accident and was not employed, after completing his or her education and before the accident, in an employment that reflected his or her education and training.
(2) Subject to subsection (3), the amount of the non-earner benefit shall be $185 for each week that the insured person is eligible to receive the benefit.
(3) If a person qualifies for a non-earner benefit under paragraph 3 of subsection (1) and more than 104 weeks have elapsed since the onset of the disability, the amount of the non-earner benefit shall be $320 for each week that the insured person continues to be eligible to receive the benefit. O. Reg. 403/96, s. 12 (1-3).
(4) The insurer may deduct the following amounts from the amount payable to an insured person as a non-earner benefit:
1. Net weekly payments for loss of income that are being received by the insured person as a result of the accident under the laws of any jurisdiction or under any income continuation benefit plan.
2. Net weekly payments for loss of income that are not being received by the insured person but are available to the insured person as a result of the accident under the laws of any jurisdiction or under any income continuation benefit plan, unless the insured person has applied to receive the payments for loss of income. O. Reg. 403/96, s. 12 (4); O. Reg. 462/96, s. 6.
(5) For the purpose of subsection (4), subsections 7 (2) and (3) apply with necessary modifications.
(6) Subject to subsection (7), the non-earner benefit is payable during the period that the insured person suffers a complete inability to carry on a normal life.
(7) The insurer,
(a) is not required to pay a non-earner benefit for the first 26 weeks after the onset of the complete inability to carry on a normal life; and
(b) is not required to pay a non-earner benefit for any period before the insured person attains 16 years of age.
(8) Sections 9 and 10 apply, with necessary modifications, to a non-earner benefit and, for that purpose, the reference in subsection 10 (1) to “the amount determined under section 7” shall be deemed to be a reference to the amount referred to in subsection (2) of this section. O. Reg. 403/96, s. 12 (5-8).
13. (1) The insurer shall pay an insured person who sustains an impairment as a result of an accident a caregiver benefit if the insured person meets all of the following qualifications:
1. At the time of the accident,
i. the insured person was residing with a person in need of care, and
ii. the insured person was the primary caregiver for the person in need of care and did not receive any remuneration for engaging in caregiving activities.
2. As a result of and within 104 weeks after the accident, the insured person suffers a substantial inability to engage in the caregiving activities in which he or she engaged at the time of the accident.
(2) The caregiver benefit shall pay for reasonable and necessary expenses incurred as a result of the accident in caring for a person in need of care.
(3) The amount of the caregiver benefit shall not exceed,
(a) for the first person in need of care,
(i) $250 per week, or
(ii) if the optional caregiver and dependant care benefit referred to in section 27 has been purchased and is applicable to the insured person, the amount fixed by the optional benefit; and
(b) for each additional person in need of care,
(i) $50 per week, or
(ii) if the optional caregiver and dependant care benefit referred to in section 27 has been purchased and is applicable to the insured person, the amount fixed by the optional benefit.
(4) The insurer is not required to pay a caregiver benefit for any period longer than 104 weeks of disability, unless, as a result of the accident, the insured person is suffering a complete inability to carry on a normal life. O. Reg. 403/96, s. 13.
PART V
MEDICAL, REHABILITATION AND ATTENDANT CARE BENEFITS
14. (1) The insurer shall pay an insured person who sustains an impairment as a result of an accident a medical benefit. O. Reg. 403/96, s. 14 (1).
(2) The medical benefit shall pay for all reasonable and necessary expenses incurred by or on behalf of the insured person as a result of the accident for,
(a) medical, surgical, dental, optometric, hospital, nursing, ambulance, audiometric and speech-language pathology services;
(b) chiropractic, psychological, occupational therapy and physiotherapy services;
(c) medication;
(d) prescription eyewear;
(e) dentures and other dental devices;
(f) hearing aids, wheelchairs or other mobility devices, prostheses, orthotics and other assistive devices;
(g) transportation for the insured person to and from treatment sessions, including transportation for an aide or attendant;
(h) other goods and services of a medical nature that the insured person requires. O. Reg. 403/96, s. 14 (2).
(3) The insurer is not liable to pay a medical benefit for goods or services that are experimental in nature. O. Reg. 403/96, s. 14 (3).
(4) The insurer is not liable to pay a medical benefit for expenses related to professional services described in clause (2) (a), (b) or (h) rendered to an insured person that exceed the maximum rate or amount of expenses established under the Guidelines applicable to the claim. O. Reg. 281/03, s. 3.
(4.1) If the Guidelines applicable to the claim establish a range of rates or amounts for expenses related to professional services rendered to an insured person,
(a) the highest rate or amount in the range shall be deemed, for the purposes of subsection (4), to be the maximum rate or amount established under the Guidelines applicable to the claim; and
(b) an insurer that is liable to pay a medical benefit for expenses related to the services described in clause (2) (a), (b) or (h) shall not pay less than the lowest amount or rate in the range unless the insured person’s claim is for less than the lowest amount or rate in the range. O. Reg. 281/03, s. 3.
(5) Subject to subsection (6), the insurer is not liable to pay a medical benefit under clause (2) (g) for expenses related to transportation unless the expenses are authorized by, and are calculated by applying the rates set out in, the Transportation Expense Guidelines published in The Ontario Gazette by the Ontario Insurance Commission or Financial Services Commission of Ontario, as they may be amended from time to time. O. Reg. 403/96, s. 14 (5); O. Reg. 303/98, s. 1 (2).
(6) The insurer is not liable to pay a medical benefit under clause (2) (g) for expenses related to,
(a) the first 50 kilometres of transportation in the insured person’s automobile to and from a treatment session if the accident occurred before April 15, 2004; or
(b) the first 50 kilometres of transportation to and from a treatment session if the accident occurred after April 14, 2004, unless the insured person sustained a catastrophic impairment as a result of the accident. O. Reg. 458/03, s. 4.
15. (1) The insurer shall pay an insured person who sustains an impairment as a result of an accident a rehabilitation benefit. O. Reg. 403/96, s. 15 (1).
(2) The rehabilitation benefit shall pay for reasonable and necessary measures undertaken by an insured person to reduce or eliminate the effects of any disability resulting from the impairment or to facilitate the insured person’s reintegration into his or her family, the rest of society and the labour market. O. Reg. 403/96, s. 15 (2).
(3) Measures to reintegrate an insured person into the labour market include measures that are reasonable and necessary to enable the person to,
(a) engage in employment that is as similar as possible to employment in which he or she engaged before the accident; or
(b) lead as normal a work life as possible. O. Reg. 403/96, s. 15 (3).
(4) In determining whether a measure is reasonable and necessary for the purpose of subsection (3), the insurer shall consider the insured person’s personal and vocational characteristics. O. Reg. 403/96, s. 15 (4).
(5) The rehabilitation benefit shall pay for all reasonable and necessary expenses incurred by or on behalf of the insured person as a result of the accident for a purpose referred to in subsection (2) for,
(a) life skills training;
(b) family counselling;
(c) social rehabilitation counselling;
(d) financial counselling;
(e) employment counselling;
(f) vocational assessments;
(g) vocational or academic training;
(h) workplace modifications and workplace devices, including communications aids, to accommodate the needs of the insured person;
(i) home modifications and home devices, including communications aids, to accommodate the needs of the insured person, or the purchase of a new home if it is more reasonable to purchase a new home to accommodate the needs of the insured person than to renovate the insured person’s existing home;
(j) vehicle modifications to accommodate the needs of the insured person, or the purchase of a new vehicle if it is more reasonable to purchase a new vehicle to accommodate the needs of the insured person than to modify an existing vehicle;
(k) transportation for the insured person to and from counselling and training sessions, including transportation for an aide or attendant;
(l) other goods and services that the insured person requires, except services provided by a case manager. O. Reg. 403/96, s. 15 (5); O. Reg. 281/03, s. 4 (1).
(6) The insurer is not liable to pay a rehabilitation benefit for expenses related to professional services described in any of clauses (5) (a) to (g) or clause (5) (l) rendered to an insured person that exceed the maximum rate or amount of expenses established under the Guidelines applicable to the claim. O. Reg. 281/03, s. 4 (2).
(6.1) If the Guidelines applicable to the claim establish a range of rates or amounts for expenses related to professional services rendered to an insured person,
(a) the highest rate or amount in the range shall be deemed, for the purpose of subsection (6), to be the maximum rate or amount established under the Guidelines applicable to the claim; and
(b) an insurer that is liable to pay a rehabilitation benefit for expenses related to the services described in any of clauses (5) (a) to (g) or clause (5) (l) shall not pay less than the lowest amount or rate in the range unless the insured person’s claim is for less than the lowest amount or rate in the range. O. Reg. 281/03, s. 4 (2).
(7) For the purpose of clause (5) (i), expenses incurred to renovate the insured person’s home shall be deemed not to be reasonable and necessary expenses if the renovations are only for the purpose of giving the insured person access to areas of the home that are not needed for ordinary living. O. Reg. 403/96, s. 15 (7).
(8) The amount of the rehabilitation benefit for the purchase of a new home shall not exceed the value of the renovations to the insured person’s existing home that would have been required to accommodate the needs of the insured person. O. Reg. 403/96, s. 15 (8).
(9) For the purpose of clause (5) (j), expenses incurred to purchase or modify a vehicle to accommodate the needs of an insured person shall be deemed not to be reasonable and necessary expenses if they are incurred within five years after the last expenses incurred for that purpose in respect of the same accident. O. Reg. 403/96, s. 15 (9).
(10) The amount of the rehabilitation benefit for the purchase of a new vehicle shall not exceed the cost of the new vehicle, less the trade-in value of the existing vehicle. O. Reg. 403/96, s. 15 (10).
(11) Subject to subsection (12), the insurer is not liable to pay a rehabilitation benefit under clause (5) (k) for expenses related to transportation unless the expenses are authorized by, and are calculated by applying the rates set out in, the Transportation Expense Guidelines published in The Ontario Gazette by the Ontario Insurance Commission or Financial Services Commission of Ontario, as they may be amended from time to time. O. Reg. 403/96, s. 15 (11); O. Reg. 303/98, s. 2 (2).
(12) The insurer is not liable to pay a rehabilitation benefit under clause (5) (k) for expenses related to,
(a) the first 50 kilometres of transportation in the insured person’s automobile to and from a counselling or training session if the accident occurred before April 15, 2004; or
(b) the first 50 kilometres of transportation to and from a counselling or training session if the accident occurred after April 14, 2004, unless the insured person sustained a catastrophic impairment as a result of the accident. O. Reg. 458/03, s. 5.
16. (1) The insurer shall pay an insured person who sustains an impairment as a result of an accident an attendant care benefit. O. Reg. 403/96, s. 16 (1).
(1.1) Despite subsection (1), no attendant care benefit is payable to an insured person whose impairment comes within the Grade I Whiplash Guideline or the Grade II Whiplash Guideline if the accident occurred after April 14, 2004. O. Reg. 458/03, s. 6 (1).
(2) The attendant care benefit shall pay for all reasonable and necessary expenses incurred by or on behalf of the insured person as a result of the accident for,
(a) services provided by an aide or attendant; or
(b) services provided by a long-term care facility, including a nursing home, home for the aged or chronic care hospital. O. Reg. 403/96, s. 16 (2).
(3) Subsection (2) does not apply to expenses for which payment may be obtained under clause 14 (2) (g), 15 (5) (k) or 24 (1) (c). O. Reg. 403/96, s. 16 (3).
(4) The monthly amount payable by the attendant care benefit shall be determined in accordance with Form 1. O. Reg. 403/96, s. 16 (4).
(5) The amount of the attendant care benefit payable in respect of an insured person shall not exceed the amount determined under the following rules:
1. If the accident occurred before October 1, 2003, the amount of the attendant care benefit payable in respect of the insured person shall not exceed,
i. $3,000 per month, if the insured person did not sustain a catastrophic impairment as a result of the accident, or
ii. $6,000 per month, if the insured person sustained a catastrophic impairment as a result of the accident.
2. If the accident occurred on or after October 1, 2003 and the optional medical, rehabilitation and attendant care benefit referred to in section 27 has not been purchased and does not apply to the insured person, the amount of the attendant care benefit payable in respect of the insured person shall not exceed,
i. $3,000 per month, if the insured person did not sustain a catastrophic impairment as a result of the accident, or
ii. $6,000 per month, if the insured person sustained a catastrophic impairment as a result of the accident.
3. If the accident occurred on or after October 1, 2003 and the optional medical, rehabilitation and attendant care benefit referred to in section 27 has been purchased and applies to the insured person, the amount of the attendant care benefit payable in respect of the insured person shall not exceed the monthly limit under subsection 27 (5). O. Reg. 281/03, s. 5; O. Reg. 458/03, s. 6 (2).
17. (1) The insurer shall pay all reasonable and necessary expenses incurred by or on behalf of an insured person as a result of the accident for services provided by a qualified case manager in accordance with a treatment plan if,
(a) the insured person sustains a catastrophic impairment as a result of the accident; or
(b) the accident occurred on or after October 1, 2003 and the optional medical, rehabilitation and attendant care benefit referred to in section 27 has been purchased and applies to the insured person. O. Reg. 281/03, s. 6.
(2) The insurer is not liable under subsection (1) to pay expenses related to professional services rendered to an insured person that exceed the maximum rate or amount of expenses established under the Guidelines applicable to the claim. O. Reg. 281/03, s. 6.
(3) If the Guidelines applicable to the claim establish a range of rates or amounts for expenses related to professional services rendered to an insured person,
(a) the highest rate or amount in the range shall be deemed, for the purpose of subsection (2), to be the maximum rate or amount established under the Guidelines applicable to the claim; and
(b) an insurer that is liable under subsection (1) to pay expenses related to the services rendered to the insured person shall not pay less than the lowest amount or rate in the range, unless the insured person’s claim is for less than the lowest amount or rate in the range. O. Reg. 281/03, s. 6.
Duration of Medical, Rehabilitation and Attendant Care Benefits
18. (1) No medical or rehabilitation benefit is payable for expenses incurred,
(a) more than 10 years after the accident, in the case of an insured person who was 15 years of age or more at the time of the accident; or
(b) after the insured person attains 25 years of age, in the case of an insured person who was less than 15 years of age at the time of the accident.
(2) No attendant care benefit is payable for expenses incurred more than 104 weeks after the accident.
(3) Subsections (1) and (2) do not apply in respect of an insured person who sustains a catastrophic impairment as a result of the accident.
(4) Subsections (1) and (2) do not apply if the optional medical, rehabilitation and attendant care benefit referred to in section 27 has been purchased and is applicable to the insured person. O. Reg. 403/96, s. 18.
Maximum Limits on Medical, Rehabilitation and Attendant Care Benefits
19. (1) The sum of the medical and rehabilitation benefits paid in respect of an insured person shall not exceed, for any one accident,
(a) $100,000; or
(b) if the insured person sustained a catastrophic impairment as a result of the accident, $1,000,000. O. Reg. 403/96, s. 19 (1).
(2) The amount of the attendant care benefit paid in respect of an insured person shall not exceed, for any one accident,
(a) $1,000,000, if the insured person sustained a catastrophic impairment as a result of the accident;
(b) nil, if the accident occurred after April 14, 2004 and the insured person sustained an impairment that comes within the Grade I Whiplash Guideline or the Grade II Whiplash Guideline; or
(c) $72,000 in any other case. O. Reg. 458/03, s. 7.
(3) If the optional medical, rehabilitation and attendant care benefit referred to in section 27 was purchased and applies to the insured person, the maximum limits fixed by the optional benefit apply and subsection (1) and clauses (2) (a) and (c) do not apply. O. Reg. 458/03, s. 7.
(4) For the purpose of subsection (1), the medical and rehabilitation benefits paid in respect of an insured person include any amount paid in respect of the insured person under section 17. O. Reg. 403/96, s. 19 (4).
PART VI
PAYMENT OF OTHER EXPENSES
20. (1) The insurer shall pay for lost educational expenses incurred by or on behalf of an insured person who sustains an impairment as a result of an accident if,
(a) at the time of the accident, the insured person was enrolled in a program of elementary, secondary, post-secondary or continuing education; and
(b) as a result of the accident, the insured person is unable to continue the program.
(2) The amount payable under this section shall not exceed $15,000.
(3) In this section,
“lost educational expenses” means expenses incurred before the accident for tuition, books, equipment or room and board in respect of the program term or program year in which the insured person was enrolled at the time of the accident, if the expenses are related to the program that the insured person is unable to continue. O. Reg. 403/96, s. 20.
21. (1) If an insured person sustains an impairment as a result of an accident, the insurer shall pay for reasonable and necessary expenses incurred by the following persons as a result of the accident in visiting the insured person during his or her treatment or recovery:
1. The spouse, children, grandchildren, parents, grandparents, brothers and sisters of the insured person.
2. An individual who was living with the insured person at the time of the accident.
3. An individual who has demonstrated a settled intention to treat the insured person as a child of the individual’s family.
4. An individual whom the insured person has demonstrated a settled intention to treat as a child of the insured person’s family. O. Reg. 403/96, s. 21 (1); O. Reg. 114/00, s. 2; O. Reg. 314/05, s. 2.
(2) No payment is required under this section for expenses incurred more than 104 weeks after the accident.
(3) Subsection (2) does not apply if the insured person sustained a catastrophic impairment as a result of the accident. O. Reg. 403/96, s. 21 (2, 3).
Housekeeping and Home Maintenance
22. (1) The insurer shall pay for reasonable and necessary additional expenses incurred by or on behalf of an insured person as a result of an accident for housekeeping and home maintenance services if, as a result of the accident, the insured person sustains an impairment that results in a substantial inability to perform the housekeeping and home maintenance services that he or she normally performed before the accident.
(2) The amount payable under this section shall not exceed $100 per week.
(3) No payment is required under this section for expenses incurred more than 104 weeks after the onset of the disability.
(4) Subsection (3) does not apply if the insured person sustained a catastrophic impairment as a result of the accident. O. Reg. 403/96, s. 22.
Damage to Clothing, Glasses, Hearing Aids, etc.
23. The insurer shall pay for all reasonable expenses incurred by or on behalf of an insured person in repairing or replacing,
(a) clothing worn by the insured person at the time of an accident that was lost or damaged as a result of the accident; or
(b) prescription eyewear, dentures, hearing aids, prostheses and other medical or dental devices that were lost or damaged as a result of an accident. O. Reg. 403/96, s. 23.
24. (1) The insurer shall pay the following expenses incurred by or on behalf of an insured person:
1. Reasonable fees charged by,
i. a health practitioner for preparing a disability certificate under section 34,
ii. a health practitioner for reviewing a treatment plan under section 38, and for approving it, if appropriate,
iii. a member of a health profession for preparing an application for approval of an assessment or examination under section 38.2,
iv. a member of a health profession for preparing an assessment of attendant care needs under section 39,
v. a health practitioner for preparing an application for a determination of catastrophic impairment under section 40.
2. Fees charged,
i. for a designated assessment of the insured person,
ii. by a health practitioner in accordance with a Pre-approved Framework Guideline for preparing a treatment confirmation form for the purposes of section 37.1,
iii. by a member of a health profession in accordance with a Pre-approved Framework Guideline for conducting an assessment or examination and preparing a report for the purposes of section 37.1.
3. Reasonable fees, other than fees referred to in paragraph 1 or subparagraph 2 iii, that are charged by a member of a health profession for conducting an assessment or examination and preparing a report, if the assessment or examination and the report are reasonably required in connection with a benefit claimed or the preparation of a treatment plan, disability certificate, assessment of attendant care needs in Form 1 or application for the determination of a catastrophic impairment and,
i. the assessment or examination and the preparation of the report,
A. relates to ancillary goods or services described in section 37.2, and
B. are services contemplated by a treatment confirmation form submitted in accordance with section 37.1, or
ii. the insured person submits the expense for approval under a treatment plan under section 38 or submits an application for approval of an assessment or examination under section 38.2. O. Reg. 281/03, s. 7 (1).
(1.1) An insurer is not required to pay an expense referred to in subparagraph 3 ii of subsection (1) if the expense is incurred,
(a) before obtaining the approval of the insurer; or
(b) before a designated assessment is conducted and the report of the person or persons who conducted the designated assessment is delivered to the insured person and the insurer, in the case where an application for approval for an assessment or examination was made under section 38.2 and denied by the insurer. O. Reg. 281/03, s. 7 (1).
(1.2) Despite subsection (1.1), the prior approval of an insurer is not required for the following:
1. An assessment or examination for the purposes of preparing a treatment plan under section 38 in circumstances in which an immediate risk of harm to the insured person or a person in the insured person’s care makes obtaining the prior approval of the insurer impractical.
2. Not more than three assessments or examinations for the purposes of preparing a treatment plan under section 38 if,
i. the insured person has not received treatment under a Pre-approved Framework Guideline,
ii. the cost of each assessment or examination does not exceed $180, and
iii. not more than one assessment or examination is done by the same person.
3. Not more than one assessment or examination for the purposes of preparing a treatment plan under section 38 if,
i. the insured person has received treatment under a Pre-approved Framework Guideline,
ii. the cost of the assessment or examination does not exceed $180, and
iii. the person conducting the assessment or examination did not provide goods or services to the insured person under a Pre-approved Framework Guideline in respect of the same accident.
4. An assessment or examination for the purposes of preparing a disability certificate under section 34, if the cost of the assessment or examination does not exceed $180.
5. An assessment or examination for the purposes of preparing an assessment of attendant care needs under section 39, but not an assessment or examination relating to an impairment that comes within a Pre-approved Framework Guideline unless the Guideline expressly states that the prior approval of the insurer is not required for the assessment or examination.
6. An assessment or examination for the purposes of determining if an insured person has a catastrophic impairment, if the insured person is hospitalized or is in a long-term care facility at the time of the assessment or examination.
7. An assessment or examination conducted after the insurer notifies the insured person that, before the assessment or examination is conducted, the insurer does not require the submission of a treatment plan under section 38 or an application for approval of an assessment or examination under section 38.2.
8. An assessment or examination conducted under the provisions of a Guideline that authorizes the assessment or examination without the prior approval of the insurer. O. Reg. 281/03, s. 7 (1).
(1.3) If the approval of an insurer is required and is requested with respect to an assessment or examination required for the purposes of preparing a treatment plan, the insurer shall give notice as to whether it will agree to pay for the assessment or examination,
(a) within two business days after receiving the request if the amount to be charged for the assessment is $180 or less; or
(b) within five business days after receiving the request if the amount to be charged is greater than $180. O. Reg. 281/03, s. 7 (1).
(1.4) A notice required under subsection (1.3) may be given verbally to the insured person, to the member of the health profession who intends to perform the assessment or examination or to both of them if, as soon as practicable afterwards, written confirmation of the notice is given to the insured person and, if the notice was given verbally to the member of the health profession, to the member of the health profession. O. Reg. 281/03, s. 7 (1).
(1.5) If an insurer fails to provide a notice required under subsection (1.3) within the time period required under that subsection, the insurer shall be deemed to have agreed to pay for the assessment or examination. O. Reg. 281/03, s. 7 (1).
(1.6) Subject to subsection (4), the insurer shall pay reasonable expenses incurred by or on behalf of an insured person for transportation expenses incurred in transporting the insured person to and from an assessment or examination referred to in subsection (1), including transportation expenses for an aide or an attendant. O. Reg. 281/03, s. 7 (1).
(2) The insurer is not liable under subsection (1) for expenses related to professional services rendered to an insured person that exceed the maximum rate or amount of expenses established under the Guidelines applicable to the claim. O. Reg. 281/03, s. 7 (1).
(2.1) If the Guidelines applicable to the claim establish a range of rates or amounts for expenses related to professional services rendered to an insured person,
(a) the highest rate or amount in the range shall be deemed, for the purpose of subsection (2), to be the maximum rate or amount established under the Guidelines applicable to the claim; and
(b) an insurer that is liable to pay expenses related to the services rendered to the insured person shall not pay less than the lowest amount or rate in the range, unless the insured person’s claim is for less than the lowest amount or rate in the range. O. Reg. 281/03, s. 7 (1).
(3) Subject to subsection (4), the insurer is not liable under subsection (1.6) to pay for expenses related to transportation unless the expenses are authorized by, and are calculated by applying the rates set out in, the Transportation Expense Guidelines published in The Ontario Gazette by the Ontario Insurance Commission or Financial Services Commission of Ontario, as they may be amended from time to time. O. Reg. 403/96, s. 24 (3); O. Reg. 303/98, s. 4 (2); O. Reg. 281/03, s. 7 (2).
(4) The insurer is not liable under subsection (1.6) to pay for expenses related to,
(a) the first 50 kilometres of transportation in the insured person’s automobile to and from an examination or assessment if the examination or assessment relates to an accident that occurred before April 15, 2004; or
(b) the first 50 kilometres of transportation to and from an examination or assessment if the examination or assessment relates to an accident that occurred after April 14, 2004, unless the insured person sustained a catastrophic impairment as a result of the accident. O. Reg. 458/03, s. 8.
(5) Vocational assessments referred to in clause 15 (5) (f) are not assessments for the purposes of this section. O. Reg. 281/03, s. 7 (4).
PART VII
DEATH AND FUNERAL BENEFITS
25. (1) The insurer shall pay a death benefit in respect of an insured person if he or she dies as result of an accident,
(a) within 180 days after the accident; or
(b) within 156 weeks after the accident, if during that period the insured person was continuously disabled as a result of the accident. O. Reg. 403/96, s. 25 (1).
(2) The death benefit shall provide for the following payments:
1. A payment to the insured person’s spouse of,
i. $25,000, or
ii. if the optional death and funeral benefit referred to in section 27 has been purchased and is applicable to the insured person, the amount fixed by the optional benefit.
2. A payment to each of the insured person’s dependants, and to each person to whom the insured person had an obligation at the time of the accident to provide support under a domestic contract or court order, of,
i. $10,000, or
ii. if the optional death and funeral benefit referred to in section 27 has been purchased and is applicable to the insured person, the amount fixed by the optional benefit.
3. If no payment is required by paragraph 1, an additional payment to the insured person’s dependants and the persons, other than a former spouse of the insured person, to whom the insured person had an obligation at the time of the accident to provide support under a domestic contract or court order, to be divided equally among the persons entitled, in an amount equal to $25,000 if the accident occurred before October 1, 2003 or, if the accident occurred on or after October 1, 2003,
i. $25,000, or
ii. if the optional death and funeral benefit referred to in section 27 has been purchased and is applicable to the insured person, the amount fixed by the optional benefit.
4. A payment of $10,000 to each former spouse of the insured person to whom the insured person was obligated at the time of the accident to provide support under a domestic contract or court order.
5. A payment of $10,000 to,
i. a person in respect of whom the insured person was a dependant at the time of the accident,
ii. the spouse of a person in respect of whom the insured person was a dependant at the time of the accident, if the spouse was the insured person’s primary caregiver at the time of the accident and the person in respect of whom the insured person was a dependant at the time of the accident dies before the insured person or within 30 days after the insured person, or
iii. the dependants of a person in respect of whom the insured person was a dependant at the time of the accident, if no payment is required by subparagraph i or ii, to be divided equally among the persons entitled. O. Reg. 403/96, s. 25 (2); O. Reg. 114/00, s. 3 (1); O. Reg. 281/03, s. 8 (1); O. Reg. 314/05, s. 3 (1-3).
(3) No payment shall be made under this section to a person who dies before the insured person or within 30 days after the insured person. O. Reg. 403/96, s. 25 (3).
(4) If at the time of the accident the insured person had more than one spouse who is entitled to a payment under this section, the payment shall be divided equally among them. O. Reg. 403/96, s. 25 (4); O. Reg. 114/00, s. 3 (2); O. Reg. 314/05, s. 3 (4).
(4.1) If at the time of the accident the insured person was a dependant in respect of more than one person who is entitled to a payment under this section, the payment shall be divided equally among the persons in respect of whom the insured person was a dependant. O. Reg. 281/03, s. 8 (2).
(5) If requested by the insurer, a person who conducts an autopsy of the insured person shall provide a copy of his or her report to the insurer. O. Reg. 403/96, s. 25 (5).
(6) In this section,
“spouse” means a person who was, at the time of the accident,
(a) a spouse, or
(b) if the accident occurred before the definition of “same-sex partner” in Part VI of the Act was repealed, a same-sex partner within the meaning of that Part as it read on January 1, 2004. O. Reg. 314/05, s. 3 (5).
26. (1) The insurer shall pay a funeral benefit in respect of an insured person who dies as a result of an accident.
(2) The funeral benefit shall pay for funeral expenses incurred in an amount not exceeding,
(a) $6,000; or
(b) if the optional death and funeral benefit referred to in section 27 has been purchased and is applicable to the insured person, the amount fixed by the optional benefit. O. Reg. 403/96, s. 26.
Description of Optional Benefits
27. (1) Every insurer shall offer the following optional benefits:
1. An optional income replacement benefit that fixes the amount referred to in subparagraph ii of paragraph 2 of subsection 7 (1) at $600, $800 or $1,000, as selected by the named insured under the policy, for the purpose of determining the weekly amount of an income replacement benefit.
2. An optional caregiver and dependant care benefit that,
i. fixes the maximum payment for expenses incurred in caring for a person in need of care at $325 per week for the first person in need of care and $75 per week for each additional person in need of care, instead of the amounts specified in subclauses 13 (3) (a) (i) and 13 (3) (b) (i), and
ii. provides for the dependant care benefit described in section 28.
3. An optional medical, rehabilitation and attendant care benefit that provides for the following maximum limits on medical, rehabilitation and attendant care benefits, instead of the limits specified in subsections 19 (1) and (2), and that provides for no limitation on the period of time for which expenses shall be paid for medical, rehabilitation and attendant care benefits:
i. The sum of the medical and rehabilitation benefits paid in respect of an insured person shall not exceed, for any one accident,
A. $1,100,000, or
B. $2,000,000, if the insured person sustained a catastrophic impairment as a result of the accident.
ii. The amount of the attendant care benefit paid in respect of an insured person shall not exceed, for any one accident,
A. $2,000,000, if the insured person sustained a catastrophic impairment as a result of the accident,
B. $1,072,000 in any case in which the insured person did not sustain as a result of the accident,
1. a catastrophic impairment, or
2. an impairment that comes within the Grade I Whiplash Guideline or the Grade II Whiplash Guideline, if the accident occurred after April 14, 2004, or
C. nil, if the accident occurred after April 14, 2004 and the insured person sustained an impairment that comes within the Grade I Whiplash Guideline or the Grade II Whiplash Guideline.
iii. Despite the limits established by subparagraphs i and ii, the overall total of the medical, rehabilitation and attendant care benefits paid in respect of an insured person for any one accident shall not exceed,
A. $1,172,000, or
B. $3,000,000, if the insured person sustained a catastrophic impairment as a result of the accident.
4. An optional death and funeral benefit that,
i. fixes the amount payable under paragraph 1 of subsection 25 (2) at $50,000, instead of the amount specified in subparagraph 1 i of subsection 25 (2),
ii. fixes the amount payable under paragraph 2 of subsection 25 (2) at $20,000, instead of the amount specified in subparagraph 2 i of subsection 25 (2),
iii. fixes the amount payable under paragraph 3 of subsection 25 (2) at $50,000 if the accident occurred on or after October 1, 2003, instead of the amount specified in subparagraph 3 i of subsection 25 (2), and
iv. fixes the maximum payment for funeral expenses at $8,000 instead of the amount specified in clause 26 (2) (a).
5. An optional indexation benefit, as described in section 29. O. Reg. 403/96, s. 27 (1); O. Reg. 114/00, s. 4 (1); O. Reg. 281/03, s. 9 (1); O. Reg. 458/03, s. 9 (1).
(2) The optional benefits referred to in subsection (1) are applicable only to,
(a) the named insured;
(b) the spouse of the named insured;
(c) the dependants of the named insured and of the named insured’s spouse; and
(d) the persons specified in the policy as drivers of the insured automobile. O. Reg. 403/96, s. 27 (2); O. Reg. 114/00, s. 4 (2); O. Reg. 314/05, s. 4.
(3) An optional benefit may be purchased at any time before an accident in respect of which a claim is made. O. Reg. 403/96, s. 27 (3).
(3.1) If a person purchases an optional benefit referred to in subsection (1), the insurer shall issue to the person the endorsement set out in Ontario Policy Change Form 47 (OPCF 47), as approved by the Commissioner of Insurance on December 3, 1996 under section 227 of the Insurance Act. O. Reg. 551/96, s. 1; O. Reg. 303/98, s. 5.
(4) For the purpose of paragraph 3 of subsection (1), the medical and rehabilitation benefits paid in respect of an insured person include any amount paid in respect of the insured person under section 17. O. Reg. 403/96, s. 27 (4).
(5) The maximum monthly attendant care benefit payable in respect of an insured person shall not exceed $6,000 if the benefit is payable in respect of an accident that occurs on or after October 1, 2003. O. Reg. 458/03, s. 9 (2).
28. (1) The dependant care benefit shall pay for reasonable and necessary additional expenses incurred by or on behalf of an insured person as a result of an accident in caring for the insured person’s dependants, if the insured person meets the following qualifications:
1. The insured person sustained an impairment as a result of the accident.
2. The insured person was employed at the time of the accident.
3. The insured person is not receiving a caregiver benefit.
(2) No payment is required under this section in respect of an expense incurred after the insured person dies.
(3) The amount payable under this section shall not exceed $75 per week for the first dependant and $25 per week for each additional dependant.
(4) The total amount payable under this section shall not exceed $150 per week. O. Reg. 403/96, s. 28.
29. (1) The optional indexation benefit shall provide that the following amounts shall be subject to annual indexation in accordance with subsections (2) and (3):
1. The weekly amount of any income replacement or non-earner benefit payable under this Regulation, without regard to any reductions made under subparagraphs i and ii of paragraph 1 of subsection 7 (1).
2. The following amounts:
i. The amounts specified in subparagraphs i and ii of paragraph 2 of subsection 7 (1).
ii. The amounts specified in subsections 12 (2) and (3).
iii. The amounts specified in subclauses 13 (3) (a) (i) and (ii) and 13 (3) (b) (i) and (ii).
iv. The amounts specified in clauses 16 (5) (a) and (b).
3. If the optional medical, rehabilitation and attendant care benefit referred to in section 27 was purchased and is applicable to the insured person, the following amounts:
i. The outstanding balance with respect to medical and rehabilitation benefits, as calculated under subsection (4).
ii. The outstanding balance with respect to attendant care benefits, as calculated under subsection (6).
iii. The outstanding balance with respect to medical, rehabilitation and attendant care benefits, as calculated under subsection (8).
4. If paragraph 3 does not apply, the following amounts:
i. The outstanding balance with respect to medical and rehabilitation benefits, as calculated under subsection (10).
ii. The outstanding balance with respect to attendant care benefits, as calculated under subsection (12). O. Reg. 403/96, s. 29 (1); O. Reg. 462/96, s. 7 (1).
(2) The indexation shall be performed on January 1 of every year following an accident to which the optional indexation benefit applies by adjusting the amount to be indexed by the percentage change in the Consumer Price Index for Canada (All Items), as published by Statistics Canada under the authority of the Statistics Act (Canada), for the period from September in the year immediately preceding the previous year to September of the previous year. O. Reg. 403/96, s. 29 (2).
(3) Subsection (2) is subject to the Optional Indexation Benefit Guidelines published in The Ontario Gazette by the Ontario Insurance Commission or Financial Services Commission of Ontario, as they may be amended from time to time, except that those guidelines shall not provide for an adjustment of the amount to be indexed by a percentage greater than the percentage change in the applicable Consumer Price Index. O. Reg. 403/96, s. 29 (3); O. Reg. 303/98, s. 6.
(4) For the purpose of subparagraph i of paragraph 3 of subsection (1), the outstanding balance with respect to medical and rehabilitation benefits is calculated by subtracting the total of medical and rehabilitation benefits paid by the insurer in the year preceding January 1 of the year to which the optional indexation benefit applies from the indexation balance calculated under subsection (5).
(5) The indexation balance for the purpose of subsection (4) is,
(a) in the first year the optional indexation benefit applies, the amount specified in sub-subparagraph A or B, as the case may be, of subparagraph i of paragraph 3 of subsection 27 (1);
(b) in each subsequent year, the outstanding balance for the previous year, as calculated under subsection (4) and indexed under subsection (2).
(6) For the purpose of subparagraph ii of paragraph 3 of subsection (1), the outstanding balance with respect to attendant care benefits is calculated by subtracting the total of attendant care benefits paid by the insurer in the year preceding January 1 of the year to which the optional indexation benefit applies from the indexation balance calculated under subsection (7).
(7) The indexation balance for the purpose of subsection (6) is,
(a) in the first year the optional indexation benefit applies, the amount specified in sub-subparagraph A or B, as the case may be, of subparagraph ii of paragraph 3 of subsection 27 (1);
(b) in each subsequent year, the outstanding balance for the previous year, as calculated under subsection (6) and indexed under subsection (2).
(8) For the purpose of subparagraph iii of paragraph 3 of subsection (1), the outstanding balance with respect to medical, rehabilitation and attendant care benefits is calculated by subtracting the total of medical, rehabilitation and attendant care benefits paid by the insurer in the year preceding January 1 of the year to which the optional indexation benefit applies from the indexation balance calculated under subsection (9).
(9) The indexation balance for the purpose of subsection (8) is,
(a) in the first year the optional indexation benefit applies, the amount specified in sub-subparagraph A or B, as the case may be, of subparagraph iii of paragraph 3 of subsection 27 (1);
(b) in each subsequent year, the outstanding balance for the previous year, as calculated under subsection (8) and indexed under subsection (2). O. Reg. 403/96, s. 29 (4-9).
(10) For the purpose of subparagraph i of paragraph 4 of subsection (1), the outstanding balance with respect to medical and rehabilitation benefits is calculated by subtracting the total of medical and rehabilitation benefits paid by the insurer in the year preceding January 1 of the year to which the optional indexation benefit applies from the indexation balance calculated under subsection (11). O. Reg. 403/96, s. 29 (10); O. Reg. 462/96, s. 7 (2).
(11) The indexation balance for the purpose of subsection (10) is,
(a) in the first year the optional indexation benefit applies, the amount specified in clause 19 (1) (a) or (b), as the case may be;
(b) in each subsequent year, the outstanding balance for the previous year, as calculated under subsection (10) and indexed under subsection (2). O. Reg. 403/96, s. 29 (11).
(12) For the purpose of subparagraph ii of paragraph 4 of subsection (1), the outstanding balance with respect to attendant care benefits is calculated by subtracting the total of attendant care benefits paid by the insurer in the year preceding January 1 of the year to which the optional indexation benefit applies from the indexation balance calculated under subsection (13). O. Reg. 403/96, s. 29 (12); O. Reg. 462/96, s. 7 (3).
(13) The indexation balance for the purpose of subsection (12) is,
(a) in the first year the optional indexation benefit applies, the amount specified in clause 19 (2) (a) or (b), as the case may be;
(b) in each subsequent year, the outstanding balance for the previous year, as calculated under subsection (12) and indexed under subsection (2). O. Reg. 403/96, s. 29 (13).
30. (1) The insurer is not required to pay an income replacement benefit, a non-earner benefit or a benefit under section 20, 21 or 22 in respect of a person who was the driver of an automobile at the time of the accident,
(a) if the driver knew or ought reasonably to have known that he or she was operating the automobile while it was not insured under a motor vehicle liability policy;
(b) if the driver was driving the automobile without a valid driver’s licence;
(c) if the driver is an excluded driver under the contract of automobile insurance; or
(d) if the driver knew or ought reasonably to have known that he or she was operating the automobile without the owner’s consent. O. Reg. 403/96, s. 30 (1).
(2) The insurer is not required to pay an income replacement benefit, a non-earner benefit or a benefit under section 20, 21 or 22,
(a) in respect of any person who has made, or who knows of, a material misrepresentation that induced the insurer to enter into the contract of automobile insurance or who intentionally failed to notify the insurer of a change in the risk material to the contract;
(b) in respect of an occupant of an automobile at the time of the accident who knew or ought reasonably to have known that the driver was operating the automobile without the owner’s consent;
(c) in respect of a person who, at the time of the accident,
(i) was engaged in an act for which the person is convicted of a criminal offence, or
(ii) was an occupant of an automobile that was being used in connection with an act for which the person is convicted of a criminal offence; or
(d) in respect of a person who is convicted under section 254 of the Criminal Code (Canada) of failing to comply with a lawful demand to provide a breath sample in connection with the accident. O. Reg. 403/96, s. 30 (2); O. Reg. 281/03, s. 10 (1).
(3) Clause (2) (b) does not prevent an excluded driver or any other occupant of an automobile driven by the excluded driver from recovering accident benefits under a motor vehicle liability policy in respect of which the excluded driver or other occupant is a named insured. O. Reg. 403/96, s. 30 (3).
(4) If a person sustains an impairment as a result of an accident and,
(a) at the time of the accident, the person was engaged in, or was an occupant of an automobile that was being used in connection with, an act for which the person is charged with a criminal offence; or
(b) the person is charged under section 254 of the Criminal Code (Canada) with failing to comply with a lawful demand to provide a breath sample in connection with the accident,
the insurer shall hold in trust any amounts payable under an income replacement benefit, a non-earner benefit or a benefit under section 20, 21 or 22 until the charge is finally disposed of, at which time the amounts and any income on the amounts,
(c) shall be returned to the insurer, if the person is found guilty of the offence or an included offence; or
(d) shall be paid to the person entitled to the payment, if the person is not found guilty of the offence or an included offence. O. Reg. 403/96, s. 30 (4).
(5) In this section,
“criminal offence” means,
(a) operating an automobile while the ability to operate the automobile is impaired by alcohol or a drug,
(b) operating an automobile while the concentration of alcohol in the operator’s blood exceeds the limit permitted by law,
(c) failing to comply with a lawful demand to provide a breath sample, or
(d) any other criminal offence, whether or not the offence is related to the operation of an automobile. O. Reg. 403/96, s. 30 (5); O. Reg. 281/03, s. 10 (2).
PART X
PROCEDURES FOR CLAIMING BENEFITS
Failure to Comply with Time Limits
31. (1) A person’s failure to comply with a time limit set out in this Part does not disentitle the person to a benefit if the person has a reasonable explanation.
(2) Subsection (1) does not apply to the time limits set out in section 51. O. Reg. 403/96, s. 31.
Notice and Application for Benefits
32. (1) A person shall notify the insurer of his or her intention to apply for a benefit under this Regulation. O. Reg. 281/03, s. 11 (1).
(1.1) A person shall notify the insurer under subsection (1) no later than,
(a) the 30th day after the circumstances arose that gave rise to the entitlement to the benefit, or as soon as practicable after that day, if those circumstances arose as a result of an accident that occurred before October 1, 2003; or
(b) the seventh day after the circumstances arose that give rise to the entitlement to the benefit, or as soon as practicable after that day, if those circumstances arose as a result of an accident that occurred on or after October 1, 2003. O. Reg. 281/03, s. 11 (1).
(2) The insurer shall promptly provide the person with,
(a) the appropriate application forms;
(b) a written explanation of the benefits available under this Regulation;
(c) information to assist the person in applying for benefits; and
(d) information on any possible elections relating to income replacement, non-earner and caregiver benefits. O. Reg. 403/96, s. 32 (2).
(3) The person shall submit an application for the benefit to the insurer within 30 days after receiving the application forms. O. Reg. 403/96, s. 32 (3).
(3.1) If an insurer receives an incomplete application for a benefit under this Regulation, the insurer shall notify the person within 14 days after receiving the incomplete application that the application is incomplete and shall indicate the information that is missing. O. Reg. 281/03, s. 11 (2).
(3.2) Subsection (3.1) applies only if the insurer, after a reasonable review of the incomplete application, is unable to determine without the missing information if a benefit is payable. O. Reg. 281/03, s. 11 (2).
(4) If a person is required by an insurer to submit an additional application in respect of a benefit that the person is receiving or may be eligible to receive, the person shall submit the additional application to the insurer within 30 days after receiving the additional application forms from the insurer. O. Reg. 403/96, s. 32 (4).
(5) If subsection (3.1) applies in respect of an incomplete application, no benefit is payable before the person provides the missing information. O. Reg. 281/03, s. 11 (2).
(6) If, in respect of an accident that occurs on or after October 1, 2003, a person fails, without a reasonable explanation, to notify an insurer under subsection (1) within the seven days set out in clause (1.1) (b), the insurer may delay determining if the person is entitled to a benefit under section 35, 38, 39 or 41 for a maximum of 45 days after the day the insurer receives the person’s application. O. Reg. 281/03, s. 11 (2).
Duty of Applicant to Provide Information
33. (1) A person applying for a benefit under this Regulation shall, within 14 days after receiving a request from the insurer, provide the insurer with the following:
1. Any information reasonably required to assist the insurer in determining the person’s entitlement to a benefit.
2. A statutory declaration as to the circumstances that gave rise to the application for a benefit.
3. The number, street and municipality where the person ordinarily resides.
4. Proof of the person’s identity. O. Reg. 403/96, s. 33 (1).
(1.1) If requested by the insurer, a person who applies for a benefit under this Regulation as a result of an accident shall submit to an examination under oath, but is not required to,
(a) submit to more than one examination under oath in respect of matters relating to the same accident; or
(b) submit to an examination under oath during a period when the person is incapable of being examined under oath because of his or her physical, mental or psychological condition. O. Reg. 281/03, s. 12 (1).
(1.2) A person is entitled to be represented at his or her own expense at the examination under oath by such counsel or other representative of his or her choice as the law otherwise permits. O. Reg. 281/03, s. 12 (1).
(1.3) The insurer shall make reasonable efforts to schedule the examination under oath for a time and location that are convenient for the person and shall give the person reasonable advance notice of the following:
1. The date and location of the examination.
2. That the person is entitled to be represented in the manner described in subsection (1.2).
3. The reason or reasons for the examination.
4. That the scope of the examination will be limited to matters that are relevant to the person’s entitlement to benefits. O. Reg. 281/03, s. 12 (1).
(1.4) The insurer shall limit the scope of the examination under oath to matters that are relevant to the person’s entitlement to benefits under this Regulation. O. Reg. 281/03, s. 12 (1).
(2) The insurer is not liable to pay a benefit in respect of any period during which the insured person failed to comply with subsection (1) or (1.1). O. Reg. 281/03, s. 12 (2).
(3) Subsection (2) does not apply in respect of a non-compliance with subsection (1.1) if,
(a) the insurer fails to comply with subsection (1.3) or (1.4); or
(b) the insurer interferes with the insured person’s right to be represented as described in subsection (1.2). O. Reg. 281/03, s. 12 (2).
(4) If an insured person who failed to comply with subsection (1) or (1.1) subsequently complies with that subsection, the insurer,
(a) shall resume payment of the benefit, if a benefit was being paid; and
(b) shall pay all amounts that were withheld during the period of non-compliance, if the insured person provides a reasonable explanation for the delay in complying with the subsection. O. Reg. 281/03, s. 12 (2).
34. (1) An insurer may require a person who claims an income replacement, non-earner or caregiver benefit, or a benefit under section 20 or 22, to furnish a certificate from a health practitioner of the person’s choice as often as is reasonably necessary.
(2) The certificate shall state the cause and nature of the impairment and an estimate of the duration of the disability in respect of which the benefit is claimed.
(3) If an insurer requires a certificate, the person shall furnish the certificate within 21 days after receiving the insurer’s request.
(4) If the person fails to comply with subsection (3), no benefit is payable for the period more than 21 days after the person received the insurer’s request and before the person furnishes the certificate. O. Reg. 403/96, s. 34.
Payment of Income Replacement, Non-earner or Caregiver Benefit
35. (1) On receiving an application for an income replacement, non-earner or caregiver benefit, an insurer shall promptly determine whether a benefit is payable. O. Reg. 403/96, s. 35 (1).
(2) If the insurer determines that a benefit is payable, the insurer shall pay the benefit to the person within 14 days after receiving the application. O. Reg. 403/96, s. 35 (2).
(3) Despite subsection (2), the insurer may delay determining whether a person is entitled to the benefit for up to 45 days from the date the insurer receives the person’s application if the person fails, without a reasonable explanation, to notify the insurer within the 30 days required under clause 32 (1.1) (a) if the application relates to an accident that occurred before October 1, 2003. O. Reg. 281/03, s. 13.
(4) An insurer that is required to pay an income replacement, non-earner or caregiver benefit shall pay the benefit at least once every second week. O. Reg. 403/96, s. 35 (4).
(5) Subsection (4) does not apply if the insurer prepays amounts owing under the benefit. O. Reg. 403/96, s. 35 (5).
Election of Income Replacement, Non-earner or Caregiver Benefit
36. (1) Only one of the following benefits may be paid to a person in respect of a period of time:
1. An income replacement benefit.
2. A non-earner benefit.
3. A caregiver benefit.
(2) If a person’s application indicates that he or she may qualify for more than one of the benefits referred to in subsection (1), the insurer shall notify the person that he or she must elect within 30 days after receiving the notice which benefit he or she wishes to receive.
(3) The insurer shall deliver the notice under subsection (2) within 14 days after receiving the person’s application. O. Reg. 403/96, s. 36.
Refusal or Stoppage of Income Replacement, Non-earner or Caregiver Benefit
37. (1) If the insurer determines that a person is not entitled or is no longer entitled to receive an income replacement, non-earner or caregiver benefit, the insurer shall give the person notice of its determination, with reasons,
(a) within 14 days after receiving an application for the benefit; or
(b) if the insurer has been paying the benefit to the person, no later than the date the next payment of the benefit is due. O. Reg. 403/96, s. 37 (1).
(2) If notice is given under clause (1) (b), the insurer shall specify in the notice a date for stopping the benefit and the insurer may stop payment of the benefit in accordance with the notice. O. Reg. 403/96, s. 37 (2).
(3) The following rules apply if notice is given under clause (1) (b) for the reason that the person no longer has a disability that entitles the person to continue to receive the benefit:
1. The date specified in the notice under subsection (2) shall be not less than 14 days after the day the person receives the notice.
2. The notice under clause (1) (b) shall inform the person that he or she has the right to require a designated assessment in accordance with section 43 by giving the insurer written notice and a disability certificate from a health practitioner under section 34, before the date specified in the notice under subsection (2).
3. Despite subsection (2), the insurer shall not stop payment of the benefit if, within 14 days after receiving the notice under clause (1) (b), the person gives the insurer written notice that he or she requires a designated assessment in accordance with section 43 and provides the disability certificate referred to in paragraph 2. O. Reg. 281/03, s. 14.
(3.1) Subsections 34 (3) and (4) do not apply where the notice given by the insurer under clause (1) (b) contains the information described in paragraph 2 of subsection (3). O. Reg. 281/03, s. 14.
(4) The insurer may stop paying a benefit to a person, after providing the person with notice of its reasons for stopping payment, if,
(a) the person undergoes a designated assessment referred to in paragraph 3 of subsection (3); and
(b) the report from the designated assessment centre states that the person no longer has a disability that entitles the person to receive the benefit. O. Reg. 281/03, s. 14.
(5) The insurer may dispute the obligation to pay a benefit in accordance with sections 279 to 283 of the Act and, pending the resolution of the dispute, the insurer shall pay the benefit if,
(a) the person undergoes a designated assessment referred to in paragraph 3 of subsection (3); and
(b) the report from the designated assessment centre states that the person continues to have a disability that entitles the person to receive the benefit. O. Reg. 281/03, s. 14.
(5.1) Paragraphs 2 and 3 of subsection (3) and subsections (4) and (5) do not apply if,
(a) the notice under clause (1) (b) relates to the entitlement of the person to receive an income replacement benefit; and
(b) the notice is given for the reason that the person is not entitled to continue to receive the benefit because the period during which the benefit is payable is limited by clause 5 (2) (d) or (e). O. Reg. 458/03, s. 10.
(6) Nothing in this section prevents a person from disputing a stoppage in the payment of a benefit in accordance with sections 279 to 283 of the Insurance Act and section 50 of this Regulation and, if it is finally determined that payment of the benefit should not have been stopped, the insurer shall,
(a) resume payment of the benefit; and
(b) pay any amounts under the benefit that were not paid. O. Reg. 403/96, s. 37 (6).
Pre-approved Framework Guidelines
37.1 (1) This section applies if an insured person,
(a) submits or intends to submit an application for a benefit in accordance with section 32; and
(b) claims medical or rehabilitation benefits in respect of an impairment that comes within a Pre-approved Framework Guideline. O. Reg. 281/03, s. 15.
(2) The insured person shall submit to the insurer, within the time specified in the Pre-approved Framework Guideline applicable to the impairment, a treatment confirmation form that satisfies the following requirements:
1. The treatment confirmation form shall be prepared by a health practitioner who is authorized by law to treat the impairment that is the subject of the form and who will be the health practitioner responsible for providing goods and services under the treatment confirmation form.
2. The treatment confirmation form shall contain details concerning the impairment and specify the Pre-approved Framework Guideline under which benefits are claimed.
3. The treatment confirmation form shall include a statement by the health practitioner who prepared the form,
i. disclosing any conflict of interest that he or she has that relates to the goods or services to be provided under the Pre-approved Framework Guideline,
ii. confirming that he or she has made reasonable inquiries to determine if any person who referred the insured person to a person who will provide goods or services under the Pre-approved Framework Guideline has a conflict of interest relating to the treatment, and
iii. disclosing any conflict of interest that a person who referred the insured person to a person who will provide goods or services under the Pre-approved Framework Guideline has that relates to the treatment.
4. The treatment confirmation form shall be signed by the insured person, unless the insurer waives this requirement. O. Reg. 281/03, s. 15.
(3) A lawyer or other representative who acts for the insured person in respect of the application for a benefit or in respect of any civil proceeding arising from the accident shall, at the time the treatment confirmation form is submitted, give the insurer and the insured person written notice disclosing any conflict of interest that the lawyer or representative has relating to the claim for benefits. O. Reg. 281/03, s. 15.
(4) If a conflict of interest is disclosed in the treatment confirmation form or by a person under subsection (3), the insurer may refuse the application. O. Reg. 281/03, s. 15.
(5) Within five business days after receiving a treatment confirmation form, the insurer shall send a notice that complies with the following rules to the insured person and to the health practitioner, acknowledging receipt of the treatment confirmation form:
1. The notice shall state whether the policy referred to in the treatment confirmation form was in force at the time of the accident.
2. If the insurer refuses the application by reason of a conflict of interest, the notice shall state the reason the application is refused, what the conflict of interest is and that the insured person may submit a new application.
3. If the treatment confirmation form includes a claim for ancillary goods or services referred to in section 37.2, the notice shall comply also with the requirements of that section. O. Reg. 281/03, s. 15.
(6) Despite subsection (4), the insurer shall not refuse an application because of a conflict of interest if there is no other person within 50 kilometres of the insured person’s residence who is able to provide the goods or services to which the conflict of interest relates. O. Reg. 281/03, s. 15.
(7) If an insured person submits an application under section 32 and a treatment confirmation form under this section in respect of an impairment and the claim is accepted by the insurer, the insurer is liable to pay benefits of a type described in section 14 or 15 in respect of the impairment only in accordance with,
(a) the Pre-approved Framework Guideline to which the treatment confirmation form relates; and
(b) the requirements of section 37.2, if that section applies in respect of the claim. O. Reg. 281/03, s. 15.
(8) If the insured person has submitted an application under section 32 to the insurer, the insurer shall pay a benefit referred to in subsection (7) within 30 days after receiving an invoice for goods or services,
(a) that have been provided under the Pre-approved Framework Guideline to which the treatment confirmation form relates; or
(b) that the insurer has agreed under section 37.2 to pay for and that have been provided. O. Reg. 281/03, s. 15.
(9) An insurer is not liable to pay benefits under more than one treatment confirmation form relating to the same Pre-approved Framework Guideline. O. Reg. 281/03, s. 15.
(10) An insured person may receive benefits under two or more Pre-approved Framework Guidelines if permitted under the Guidelines. O. Reg. 281/03, s. 15.
(11) An insured person shall submit an amended treatment confirmation form if, during the course of treatment under a Pre-approved Framework Guideline, he or she changes the health practitioner who is responsible for providing goods and services under the treatment confirmation form. O. Reg. 281/03, s. 15.
(12) The insurer is liable to pay for goods and services under an amended treatment confirmation form only to the extent the goods and services have not already been provided under the Pre-approved Framework Guideline. O. Reg. 281/03, s. 15.
(13) Sections 42 and 43 do not apply to a claim for payment for goods and services provided under a Pre-approved Framework Guideline. O. Reg. 281/03, s. 15.
(14) If goods or services available under a Pre-approved Framework Guideline are not provided within the times specified in the applicable Guideline, any claim for medical or rehabilitation benefits to which the Guideline would otherwise apply shall, subject to section 37.2, be submitted in accordance with section 38. O. Reg. 281/03, s. 15.
(15) If a court or arbitrator determines in any dispute about an insured person’s entitlement to medical or rehabilitation benefits or related assessments or examinations that a Pre-approved Framework Guideline applies to the insured person and the insured person received benefits or underwent assessments or examinations under the Pre-approved Framework Guideline,
(a) the benefits shall be deemed to have been reasonable and necessary for the purposes of sections 14 and 15; and
(b) the assessments and examinations shall be deemed to have been reasonably required for the purposes of section 24. O. Reg. 281/03, s. 15.
37.2 (1) In this section, ancillary goods or services, in respect of an impairment to which a Pre-approved Framework Guideline applies, are goods or services for which the Guideline,
(a) requires the insurer’s approval; and
(b) permits a claim to be made in a treatment confirmation form under section 37.1. O. Reg. 281/03, s. 15.
(2) If a treatment confirmation form under section 37.1 includes a claim for ancillary goods or services, the following rules apply:
1. If the insurer does not agree to pay for all of the ancillary goods and services claimed in the treatment confirmation form, the insurer shall require the insured person to be assessed by a designated assessment centre in accordance with section 43 in respect of the ancillary goods and services the insurer will not pay for.
2. The notice given by the insurer under subsection 37.1 (5) shall state,
i. what ancillary goods and services, if any, that the insurer will pay for,
ii. what ancillary goods and services the insurer will not pay for and the reasons why the insurer will not pay for them, and
iii. that the insurer requires the insured person to be assessed by a designated assessment centre in accordance with section 43 in respect of the ancillary goods and services the insurer will not pay for. O. Reg. 281/03, s. 15.
(3) Despite subsection (2), no designated assessment is required if, within two business days after receiving the notice referred to in that subsection, the insured person gives the insurer written notice that he or she will not make any claim in respect of the goods and services for which the insurer has indicated it will not pay. O. Reg. 281/03, s. 15.
(4) If the insurer fails, within the time required under subsection 37.1 (5), to comply with the requirements of paragraph 2 of subsection (2) or fails to give the notice under subsection 37.1 (5), the insurer shall pay for all ancillary goods and services delivered under the treatment confirmation form. O. Reg. 281/03, s. 15.
(5) The following rules apply in respect of an expense for or relating to an ancillary good or service, subject to the determination of a dispute relating to the expense in accordance with sections 279 to 283 of the Act:
1. If a report from a designated assessment centre states that, in the opinion of the person or persons who conducted the designated assessment, the expense is reasonable and necessary for the insured person’s treatment or rehabilitation, the insurer shall pay the expense.
2. If a report from a designated assessment centre does not state that, in the opinion of the person or persons who conducted the designated assessment, the expense is reasonable and necessary for the insured person’s treatment or rehabilitation, the insurer is not required to pay the expense.
3. If a report from a designated assessment centre states that, in the opinion of the person or persons who conducted the designated assessment, the expense in respect of an assessment or examination is reasonably required in relation to the benefit claimed, the insurer shall pay the expense.
4. If a report from a designated assessment centre does not state that, in the opinion of the person or persons who conducted the designated assessment, an expense in respect of an assessment or examination is reasonably required in relation to the benefit claimed, the insurer is not required to pay the expense. O. Reg. 281/03, s. 15.
Medical and Rehabilitation Benefits
38. (1) Subject to subsection (2.1), this section applies to,
(a) any claim for medical or rehabilitation benefits other than,
(i) a claim payable under section 37.1, and
(ii) a claim for ancillary goods and services referred to in section 37.2; and
(b) applications for assessments or examinations under subparagraph 3 ii of subsection 24 (1) that are submitted with a treatment plan under subsection (2). O. Reg. 281/03, s. 16 (1).
(1.1) An insured person shall submit an application for a medical or rehabilitation benefit to the insurer before incurring any expense in respect of the benefit or an assessment or examination to which this section applies. O. Reg. 281/03, s. 16 (1).
(2) An application under this section must be signed by the insured person, unless the insurer waives that requirement, and must include, unless section 38.1 applies,
(a) a treatment plan prepared by a member of a health profession; and
(b) a statement by a health practitioner approving the treatment plan referred to in clause (a) and stating that he or she is of the opinion,
(i) that the expenses contemplated by the treatment plan are reasonable and necessary for the insured person’s treatment or rehabilitation, and
(ii) that the impairment sustained by the insured person does not come within a Pre-approved Framework Guideline. O. Reg. 281/03, s. 16 (2).
(2.1) An insurer may refuse to accept a treatment plan under this section that provides for goods or services to be received in respect of any period during which the insured person is entitled to receive goods or services under a Pre-approved Framework Guideline, unless the Guideline allows the insured person to receive both, and the insurer’s refusal is final and not subject to review. O. Reg. 281/03, s. 16 (2).
(2.2) Nothing in subsection (2.1) prevents an insured person, while receiving goods or services under a Pre-approved Framework Guideline, from submitting a treatment plan applicable to a period other than the period referred to in that subsection. O. Reg. 281/03, s. 16 (2).
(3) The treatment plan shall include a statement by the member of a health profession who prepared the plan,
(a) disclosing any conflict of interest that he or she has relating to the treatment plan;
(b) indicating that he or she has made reasonable inquiries to determine whether any person who referred the insured person to a person who will provide goods or services contemplated by the treatment plan has a conflict of interest relating to the treatment plan; and
(c) disclosing any conflict of interest that a person who referred the insured person to a person who will provide goods or services contemplated by the treatment plan has relating to the treatment plan. O. Reg. 403/96, s. 38 (3).
(3.1) Despite subsections (1.1), (2) and (3), if an insured person incurs expenses in respect of which a medical or rehabilitation benefit may be payable, other than for expenses payable under a Pre-approved Framework Guideline, without complying with subsection (1.1), (2) or (3), the insured person shall submit to the insurer an application for payment of the expenses that complies with subsections (2) and (3) within 30 days after incurring the expenses. O Reg. 281/03, s. 16 (3).
(4) A lawyer or other representative who acts for the insured person in respect of the application or in respect of any civil proceeding arising from the accident shall, at the time the application is submitted, give the insurer and the insured person written notice disclosing any conflict of interest that the lawyer or other representative has relating to the treatment plan. O. Reg. 403/96, s. 38 (4).
(5) If a conflict of interest is disclosed under subsection (3) or (4), the insurer may, within 14 days after receiving the application, give the insured person notice that the application is refused and that the insured person may submit a new application. O. Reg. 403/96, s. 38 (5).
(6) Subsection (5) does not apply if there is no other person within 50 kilometres of the insured person’s residence who is able to provide the goods or services from which the conflict of interest arises. O. Reg. 403/96, s. 38 (6).
(7) On receiving the application, the insurer shall promptly determine whether the insurer is required to pay for the goods and services contemplated by the treatment plan. O. Reg. 403/96, s. 38 (7).
(8) If no notice is given under subsection (5), the insurer shall give the insured person one of the following notices:
1. A notice disclosing if the insurer has a conflict of interest relating to the treatment plan and stating,
i. what goods and services, if any, contemplated by the treatment plan that the insurer will pay for, and
ii. what goods and services, if any, contemplated by the treatment plan that the insurer will not pay for.
2. A notice stating that the insurer rejects the treatment plan on the basis that the insured person has an impairment to which a Pre-approved Framework Guideline applies. O. Reg. 281/03, s. 16 (4).
(8.1) A notice under subsection (8) must be given,
(a) within 14 days after the insurer receives the application, in the case of a notice described in paragraph 1 of subsection (8); or
(b) within five business days after the insurer receives the application, in the case of a notice described in paragraph 2 of subsection (8). O. Reg. 281/03, s. 16 (4).
(8.2) If the insurer fails to give a notice under subsection (8) in accordance with subsection (8.1), the following rules apply:
1. In the case of a notice under paragraph 2 of subsection (8),
i. the insurer cannot reject the treatment plan on the basis that the insured person has an impairment to which a Pre-approved Framework Guideline applies, and
ii. the insurer shall give a notice described in paragraph 1 of subsection (8) in accordance with subsection (8.1).
2. In the case of a notice under paragraph 1 of subsection (8) or a notice required under that paragraph by reason of subparagraph 1 ii of this subsection, the insurer shall pay for all goods and services provided under the treatment plan that relate to the period starting the day after the day the insurer was required to give the notice and ending on the day the insurer gives the notice. O. Reg. 281/03, s. 16 (4).
(9) If the insurer discloses a conflict of interest relating to the treatment plan, the insured person may, within 14 days after receiving the notice under paragraph 1 of subsection (8), withdraw the application and submit a new application. O. Reg. 403/96, s. 38 (9); O. Reg. 281/03, s. 16 (5).
(10) Subsection (9) does not apply if there is no other person within 50 kilometres of the insured person’s residence who is able to provide the goods or services from which the conflict of interest arises. O. Reg. 403/96, s. 38 (10).
(11) If the application is not withdrawn under subsection (9), the insurer shall pay for goods and services the insurer agreed to pay for in the notice under paragraph 1 of subsection (8) within 30 days after receiving an invoice for them. O. Reg. 281/03, s. 16 (6).
(12) If the notice under paragraph 1 of subsection (8) does not indicate that the insurer will pay for all the goods and services contemplated by the treatment plan,
(a) the insurer shall require the insured person to be assessed by a designated assessment centre in accordance with section 43 in respect of the goods and services the insurer will not pay for; and
(b) the insurer shall include in the notice under paragraph 1 of subsection (8),
(i) a statement of the insurer’s reasons for not agreeing to pay for all goods and services contemplated by the treatment plan, and
(ii) notice that the insurer requires the insured person to be assessed by a designated assessment centre in accordance with section 43. O. Reg. 281/03, s. 16 (6).
(12.1) If an insurer gives a notice described in paragraph 2 of subsection (8),
(a) the insurer shall require the insured person to be assessed in respect of the goods and services by a designated assessment centre; and
(b) the insurer shall include in the notice,
(i) a statement specifying the Pre-approved Framework Guideline applicable to the insured person, and
(ii) notice that the insurer requires the insured person to be assessed by a designated assessment centre. O. Reg. 281/03, s. 16 (6).
(12.2) If an insurer gives notice described in paragraph 2 of subsection (8), the insured person may submit a treatment confirmation form under section 37.1 and receive goods and services in accordance with the Pre-approved Framework Guideline referred to in subclause (12.1) (b) (i), pending the determination of the designated assessment referred to in subclause (12.1) (b) (ii). O. Reg. 281/03, s. 16 (6).
(12.3) If appropriate, the treatment confirmation form referred to in subsection (12.2) may include a claim for ancillary goods and services under section 37.2. O. Reg. 281/03, s. 16 (6).
(13) Despite clause (12) (a), no designated assessment shall be required if, within five business days after receiving the notice under subclause (12) (b) (ii), the insured person gives the insurer written notice that he or she will not make any claim in respect of the goods or services that the insurer has stated it will not pay for. O. Reg. 281/03, s. 16 (7).
(14) The following rules apply in respect of an expense for or relating to goods or services the insurer has not agreed to pay for, subject to the determination of a dispute relating to the expense in accordance with sections 279 to 283 of the Act:
1. If a report from the designated assessment centre states that, in the opinion of the person or persons who conducted the designated assessment, an expense claimed under section 14 or 15 is reasonable and necessary for the insured person’s treatment or rehabilitation, or in the case of an assessment or examination under subparagraph 3 ii of subsection 24 (1), that the expense is reasonably required in relation to the benefit claimed, the insurer shall pay the expense.
2. If a report from the designated assessment centre does not state that, in the opinion of the person or persons who conducted the designated assessment, an expense claimed under section 14 or 15 is reasonable and necessary for the insured person's treatment or rehabilitation, or in the case of an assessment or examination under subparagraph 3 ii of subsection 24 (1), that the expense is reasonably required in relation to the benefit claimed, the insurer is not required to pay the expense.
3. If a report from the designated assessment centre states that, in the opinion of the person or persons who conducted the designated assessment, the insured person has an impairment to which a Pre-approved Framework Guideline applies, the insurer may reject the treatment plan and may treat the application for benefits as an application under section 37.1.
4. If a report from the designated assessment centre states that, in the opinion of the person or persons who conducted the designated assessment, the insured person does not have an impairment to which a Pre-approved Framework Guideline applies, the insurer shall give the insured person a notice described in paragraph 1 of subsection (8). O. Reg. 281/03, s. 16 (7).
(15) Despite subsection (12), an insurer shall not require a designated assessment, and shall not give the notice referred to in subclause (12) (b) (ii), in respect of a claim for the following expenses:
1. Expenses for assistive devices partially paid for by the Ministry of Health, including wheelchairs or other mobility devices, prostheses and orthotics.
2. Expenses for prescription eyewear, hearing aids, or dentures or other dental devices.
3. Expenses for transportation to or from counselling sessions, training sessions, or treatment sessions, including transportation for an aide or attendant.
4. Labour market re-entry expenses payable by the insurer until a dispute over whether a benefit is payable under the Workplace Safety and Insurance Act, 1997 is resolved. O. Reg. 403/96, s. 38 (15); O. Reg. 281/03, s. 16 (8, 9).
(16), (17) Revoked: O. Reg. 281/03, s. 16 (10).
(18) Despite subsection (1.1), if the insurer receives an application described in subsection (3.1), the insurer shall, within 30 days after receiving the application,
(a) pay the expenses; or
(b) give the insured person notice of its reasons for not paying the expenses. O. Reg. 403/96, s. 38 (18); O. Reg. 281/03, s. 16 (11).
(19) If, after giving notice under subparagraph 1 i of subsection (8), it comes to the attention of the insurer that a person described in subsection (3) or (4) has a conflict of interest relating to the treatment plan, the insurer may give the insured person notice requiring the insured person, within 14 days after receiving the notice, to amend the treatment plan to remove the conflict of interest. O. Reg. 403/96, s. 38 (19); O. Reg. 281/03, s. 16 (12).
(20) If the insured person does not comply with a notice under subsection (19), the insurer is not required to pay for any further expenses for goods or services from which the conflict of interest arises. O. Reg. 403/96, s. 38 (20).
(21) Subsection (20) does not apply if there is no other person within 50 kilometres of the insured person’s residence who is able to provide the goods or services from which the conflict of interest arises. O. Reg. 403/96, s. 38 (21).
(22)-(25) Revoked: O. Reg. 281/03, s. 16 (13).
38.1 (1) This section applies to a claim for a medical or rehabilitation benefit under section 38 if the insurer gives the insured person a notice informing the insured person that the insurer will pay the expenses without the submission of a treatment plan under that section. O. Reg. 281/03, s. 17.
(2) If the insurer gives the insured person a notice under subsection (1),
(a) the notice shall describe the expenses that the insurer will pay without the submission of a treatment plan and shall specify,
(i) the types of expenses,
(ii) any restrictions on the amount of the expenses, and
(iii) any restrictions on when the expenses may be incurred;
(b) the insurer shall pay expenses described in the notice within 30 days after receiving an invoice for them; and
(c) if there is a dispute about whether, for the purpose of subsection 14 (2) or 15 (5), an expense described in the notice is reasonable or necessary, the insurer shall pay the expense pending resolution of the dispute in accordance with sections 279 to 283 of the Act. O. Reg. 281/03, s. 17.
(3) The insurer shall give the insured person a notice disclosing any conflict of interest that the insurer has relating to any person who will provide goods or services to whom the insured person is referred by the insurer. O. Reg. 281/03, s. 17.
(4) Every member of a health profession who refers an insured person to a person who will provide goods or services in respect of which a medical or rehabilitation benefit will be paid by an insurer under this section shall give the insurer and the insured person written notice disclosing any conflict of interest that the member of the health profession has relating to the goods or services. O. Reg. 281/03, s. 17.
(5) If a conflict of interest is disclosed under subsection (4), the insurer may give the insured person a notice requiring the insured person to submit a treatment plan to the insurer under section 38 and, if a notice is given under this subsection,
(a) the insurer is relieved of any obligation under this section to pay expenses other than expenses incurred before the notice was given;
(b) subsections (1) to (4) do not apply; and
(c) the insured person may submit an application and treatment plan under section 38. O. Reg. 281/03, s. 17.
38.2 (1) This section applies to an application for approval of an assessment or examination referred to in subparagraph 3 ii of subsection 24 (1), unless the application is submitted with a treatment plan under section 38. O. Reg. 281/03, s. 17.
(2) The application shall include a statement by the member of a health profession who is to conduct the assessment or examination,
(a) disclosing any conflict of interest that he or she has relating to the assessment or examination to which the application relates;
(b) indicating that he or she has made reasonable inquiries to determine whether any person who referred the insured person to him or her has a conflict of interest relating to the assessment or examination and, if there is a conflict of interest, disclosing the conflict of interest that the person has; and
(c) stating that the assessment or examination is reasonably required in relation to a benefit. O. Reg. 281/03, s. 17.
(3) A lawyer or other representative who acts for the insured person in respect of the application or with respect to any civil proceeding arising from the accident shall, at the time the application is submitted, give the insurer and the insured person written notice disclosing any conflict of interest that the lawyer or other representative has relating to the application. O. Reg. 281/03, s. 17.
(4) If a conflict of interest is disclosed under subsection (2) or (3), the insurer may refuse the application and, within two business days after receiving the application, give the insured person notice that the application is refused and that the insured person may submit a new application. O. Reg. 281/03, s. 17.
(5) Despite subsection (4), the insurer shall not refuse the application because of a conflict of interest if there is no other person within 50 kilometres of the insured person’s residence who is able to conduct the assessment or examination. O. Reg. 281/03, s. 17.
(6) If the insurer has not refused the application under subsection (4), the insurer shall, within the applicable time period under subsection 24 (1.3), determine whether the insurer is required to pay for any assessment or examination to which the application relates and shall give the insured person a notice,
(a) stating which assessments or examinations in the application that the insurer will or will not pay for;
(b) specifying the insurer’s reasons for not agreeing to pay for any assessment or examination to which the application relates;
(c) requiring the insured person to be assessed by a designated assessment centre in accordance with section 43, if the insurer states in the notice that it will not pay for an assessment or examination to which the application relates; and
(d) disclosing any conflict of interest that the insurer has relating to any assessment or examination to which the application relates. O. Reg. 281/03, s. 17.
(7) If the insurer determines that it is not required to pay for any assessment or examination to which the application relates, the insurer shall require the insured person to be assessed in respect of the requirement for the assessment or examination by a designated assessment centre in accordance with section 43. O. Reg. 281/03, s. 17.
(8) Despite clause (6) (c) and subsection (7), no designated assessment shall be required in respect of an assessment or examination that the insurer has stated it will not pay for if, within two business days after receiving the notice under subsection (6), the insured person gives the insurer written notice that he or she will not make any claim in respect of the assessment or examination. O. Reg. 281/03, s. 17.
(9) If the insurer does not refuse the application under subsection (4) but fails to give the notice as required under subsection (6), the insurer shall pay for all assessments and examinations to which the application relates. O. Reg. 281/03, s. 17.
(10) If, in a notice under subsection (6), the insurer discloses a conflict of interest relating to an assessment or examination, the insured person may withdraw the application and submit a new application within two business days after receiving the notice from the insurer. O. Reg. 281/03, s. 17.
(11) Despite subsection (10), the insured person shall not withdraw the application or submit a new application if there is no other person within 50 kilometres of the insured person’s residence who is able to conduct the assessment or examination. O. Reg. 281/03, s. 17.
(12) If the application is not withdrawn under subsection (10), the insurer shall pay for all assessments and examinations it agreed to pay for in the notice under subsection (6) and shall make each payment within 30 days after receiving an invoice for the cost of the assessment or examination. O. Reg. 281/03, s. 17.
(13) The following rules apply in respect of an assessment or examination that the insurer has not agreed to pay for, subject to the determination of a dispute relating to the expense in accordance with sections 279 to 283 of the Act:
1. If a report from a designated assessment centre states that, in the opinion of the person or persons who conducted the designated assessment, the assessment or examination to which the application relates is reasonably required in relation to the benefit claimed, the insurer shall pay for the assessment or examination.
2. If a report from a designated assessment centre does not state that, in the opinion of the person or persons who conducted the designated assessment, the assessment or examination is reasonably required in relation to the benefit claimed, the insurer is not required to pay for the assessment or examination. O. Reg. 281/03, s. 17.
(14) If, after giving a notice under subsection (6) in which the insurer agrees to pay for an assessment or examination, it comes to the insurer’s attention that a person described in subsection (2) or (3) has a conflict of interest relating to the assessment or examination, the insurer may give the insured person notice requiring the insured person, within five business days after receiving the notice, to amend the application so that no conflict of interest will arise. O. Reg. 281/03, s. 17.
(15) If the insured person does not amend the application as required under subsection (14), the insurer is not required to pay for the assessment or examination referred to in that subsection. O. Reg. 281/03, s. 17.
(16) Subsection (14) does not apply if there is no other person within 50 kilometres of the insured person’s residence who is able to conduct the assessment or examination to which the conflict of interest relates. O. Reg. 281/03, s. 17.
38.3 (1) For the purposes of sections 37.1, 38, 38.1 and 38.2,
(a) a person has a conflict of interest relating to the provision of goods or services if,
(i) the person or a related person may receive a financial benefit, directly or indirectly, as a result of the provision, by the related person or another person, of the goods or services, and
(ii) the person who may receive the financial benefit is not the employee of the person who will provide the goods or services and does not have a contract with the person who will provide the goods or services or under which goods or services of that kind are provided; and
(b) an insurer has a conflict of interest relating to the provision of goods or services to an insured person if the insurer may receive a financial benefit, directly or indirectly, as a result of the provision of the goods or services. O. Reg. 281/03, s. 17.
(2) A related person, in respect of a person who is not a corporation, is an individual who is,
(a) the spouse of the person;
(b) connected with the person by blood relationship or adoption; or
(c) connected by blood relationship to the spouse of the person. O. Reg. 281/03, s. 17; O. Reg. 314/05, s. 5.
(3) For the purposes of subsection (2),
(a) persons are connected by blood relationship if one is the child or other descendant of the other or is the brother or sister of the other; and
(b) persons are connected by adoption if one has been adopted, either legally or in fact, as the child of the other or as a child of a person who is connected by blood relationship, otherwise than as brother or sister, to the other. O. Reg. 281/03, s. 17.
39. (1) Within 14 days after receiving an application for an attendant care benefit, an insurer shall,
(a) give the insured person notice that it has approved the application, if the insurer determines that it is required to pay for the expenses described in the application; or
(b) give the insured person notice that the insurer requires the insured person to furnish an assessment of attendant care needs in Form 1 prepared by a member of a health profession who is authorized by law to treat the person’s impairment. O. Reg. 403/96, s. 39 (1); O. Reg. 281/03, s. 18 (1).
(2) If the application is for an attendant care benefit in respect of expenses that are of a continuing nature, the insurer may require an assessment of attendant care needs described in clause (1) (b) to be furnished as often as is reasonably necessary. O. Reg. 403/96, s. 39 (2); O. Reg. 281/03, s. 18 (2).
(3) If the insurer is required to pay the benefit, it shall begin payment of the benefit within 30 days after receiving the application or, if the insurer has required an assessment of attendant care needs in Form 1, within 14 days after receiving Form 1. O. Reg. 281/03, s. 18 (3).
(4) If the insurer determines that an insured person is not entitled to receive an attendant care benefit, the insurer shall require the person to undergo a designated assessment in accordance with section 43 and shall give the person notice of its determination and the requirement for the designated assessment, with reasons,
(a) within 14 days after receiving the application; or
(b) within 14 days after receiving the assessment of attendant care needs in Form 1, if the insurer required an assessment of attendant care needs under this section. O. Reg. 281/03, s. 18 (3).
(5) Revoked: O. Reg. 281/03, s. 18 (3).
(6) If a designated assessment is required under subsection (4), the insurer shall pay the insured person the attendant care benefit pending receipt of the report of the designated assessment centre. O. Reg. 403/96, s. 39 (6); O. Reg. 281/03, s. 18 (4).
(7) If an insured person is receiving an attendant care benefit and the insurer determines that the person is no longer entitled to receive the benefit or that the amount of the benefit should be reduced, the insurer shall require the person to undergo a designated assessment in accordance with section 43 and shall give the person notice of its determination and the requirement for the designated assessment, with reasons, no later than the date the next payment of the benefit is due. O. Reg. 281/03, s. 18 (5).
(8) If an insured person who is receiving an attendant care benefit submits an application to the insurer to increase the amount of the benefit, and the insurer determines that the person is not entitled to receive an increased amount, the insurer shall require the person to undergo a designated assessment in accordance with section 43 and shall give the person notice of its determination and the requirement for the designated assessment, with reasons, within 14 days after the application is received. O. Reg. 281/03, s. 18 (5).
(9) If a designated assessment is required under subsection (7) or (8), the insurer shall, pending receipt of the report of the designated assessment centre, continue to pay the insured person the attendant care benefit in the amount that was being paid before the notice under that subsection was given. O. Reg. 281/03, s. 18 (5).
(10) The determination by the designated assessment centre is binding on the insured person and the insurer in respect of the attendant care benefit, subject to the determination of a dispute in accordance with sections 279 to 283 of the Act. O. Reg. 281/03, s. 18 (5).
(11) Despite subsections (7) and (8), if more than 104 weeks have elapsed since the accident, the insurer shall not require a designated assessment of the insured person and the insured person shall not submit an application to the insurer to increase the amount of the benefit unless at least 52 weeks have elapsed since the insured person was last assessed by a designated assessment centre. O. Reg. 281/03, s. 18 (5).
(12) The insured person and the insurer may agree at any time that the insured person be assessed in accordance with section 43. O. Reg. 281/03, s. 18 (5).
(13) If the insurer determines that, pursuant to subsection 18 (2), a person is not entitled to receive an attendant care benefit,
(a) subsections (4), (7), (8) and (11) do not apply; and
(b) if the insurer has been paying an attendant care benefit to the person, the insurer shall not stop payment of the benefit unless it gives the person notice of its determination, with reasons, at least 14 days before the last payment of the benefit. O. Reg. 281/03, s. 18 (5).
Determination of Catastrophic Impairment
40. (1) An insured person who sustains an impairment as a result of an accident may apply to the insurer for a determination of whether the impairment is a catastrophic impairment. O. Reg. 403/96, s. 40 (1).
(2) The insurer shall, within 30 days after it receives the application,
(a) determine that the impairment is a catastrophic impairment and give the insured person notice of the determination;
(b) determine that the impairment is not a catastrophic impairment and give the insured person notice of the determination, including the reasons for the determination; or
(c) give the insured person notice that the insurer requires the insured person to be assessed by a designated assessment centre in accordance with section 43. O. Reg. 403/96, s. 40 (2).
(3) If the insured person receives a notice under clause (2) (b) and the insured person disputes the insurer’s determination, the insured person may require that he or she be assessed by a designated assessment centre in accordance with section 43. O. Reg. 403/96, s. 40 (3).
(3.1) Despite clause 19 (2) (a), if an application under subsection (1) is made within 104 weeks after the accident and a designated assessment is required under this section, the insurer shall continue to pay the insured person the attendant care benefit in the amount that was being paid before the notice under clause (2) (c) or subsection (3) was given, pending receipt of the report from the designated assessment centre. O. Reg. 281/03, s. 19.
(4) The determination by the designated assessment centre is binding on the insured person and the insurer, subject to the determination of a dispute, in accordance with sections 279 to 283 of the Insurance Act, relating to whether the impairment is a catastrophic impairment. O. Reg. 403/96, s. 40 (4).
41. (1) If a person is entitled to a death benefit, a funeral benefit or a benefit under Part VI, the insurer shall pay the benefit within 30 days after the insurer receives the application for the benefit.
(2) If the insurer refuses to pay a benefit referred to in subsection (1), the insurer shall give the person notice of the reasons for the refusal within 30 days after the insurer receives the application for the benefit. O. Reg. 403/96, s. 41.
42. (1) For the purpose of determining whether an insured person is entitled to a benefit for which an application is made, an insurer may give the insured person notice requiring the insured person to be examined by one or more persons specified by the insurer, each of whom is a member of a health profession or a person with expertise in vocational rehabilitation. O. Reg. 281/03, s. 20 (1).
(1.1) Subsection (1) does not apply in respect of an application,
(a) for a benefit that is subject to section 37.1 or 37.2;
(b) for a funeral benefit or death benefit; or
(c) for a medical or rehabilitation benefit under section 14 or 15 unless the claim for the benefit is the subject of proceedings under sections 279 to 284 of the Act. O. Reg. 281/03, s. 20 (1).
(2) The notice shall state the reasons why the insurer requires the examination and shall specify a date for the examination that is at least five business days after the person receives the notice. O. Reg. 281/03, s. 20 (2).
(3) The insurer may require examinations as often as is reasonably necessary. O. Reg. 403/96, s. 42 (3).
(4) The insurer shall make reasonable efforts to schedule the examination for a time that is convenient for the insured person. O. Reg. 281/03, s. 20 (3).
(5) For the purpose of the examination,
(a) the insured person shall provide the person or persons who conduct the examination with such information as is reasonably necessary; and
(b) the insured person shall submit to any reasonable physical, psychological, mental and functional examinations requested by the person or persons who conduct the examination. O. Reg. 403/96, s. 42 (5).
(6) The person or persons who conduct the examination shall prepare a report and provide a copy of the report to the insurer. O. Reg. 403/96, s. 42 (6).
(7) An insurer that receives a report under subsection (6) shall provide the insured person with a copy of the report within five business days. O. Reg. 403/96, s. 42 (7); O. Reg. 281/03, s. 20 (4).
(8) If an insured person fails or refuses to submit to an examination required by the insurer under this section or fails to comply with subsection (5),
(a) the insurer may stop payment of the benefit related to the examination until the person submits to the examination or complies with subsection (5); and
(b) no benefit is payable for the period after the person has failed to attend the examination or failed to comply with subsection (5) and before the insured person submits to an examination under subsection (1) and complies with subsection (5). O. Reg. 403/96, s. 42 (8); O. Reg. 281/03, s. 20 (5).
(9) If a person subsequently submits to an examination under subsection (1) or complies with subsection (5), the insurer,
(a) shall resume payment of the benefit; and
(b) shall pay all amounts that were withheld during the period of non-compliance, if the insured person provides a reasonable explanation for not attending the examination or not complying with subsection (5). O. Reg. 281/03, s. 20 (6).
(10) No person who is member of a health profession or who has expertise in vocational rehabilitation shall examine an insured person on behalf of an insurer for the purposes of determining whether an insured person is entitled to a benefit except in accordance with this section. O. Reg. 281/03, s. 20 (6).
43. (1) The following rules apply if a designated assessment is required under this Regulation:
1. The insurer shall notify the designated assessment centre within five business days.
2. The insured person and the insurer shall provide the person or persons who will conduct the designated assessment with such information as is reasonably necessary, within the same period of five business days referred to in paragraph 1.
3. The designated assessment centre shall promptly notify the insured person and arrange for the designated assessment.
4. The insured person shall submit to all reasonable physical, psychological, mental and functional examinations requested by the person or persons who conduct the designated assessment. O. Reg. 281/03, s. 21.
(2) The following rules apply if an insured person does not submit to a designated assessment arranged under subsection (1) or fails to comply with paragraph 2 or 4 of subsection (1):
1. The insurer may stop payment of the benefit related to the designated assessment until the insured person submits to the designated assessment and complies with paragraphs 2 and 4 of subsection (1).
2. No benefit is payable for the period after the insured person fails to submit to the designated assessment or fails to comply with paragraph 2 or 4 of subsection (1) and before the insured person subsequently submits to an examination under subsection (1) and complies with paragraphs 2 and 4 of subsection (1). O. Reg. 281/03, s. 21.
(3) If an insured person subsequently submits to a designated assessment and is in compliance with paragraphs 2 and 4 of subsection (1), the insurer,
(a) shall resume payment of the benefit; and
(b) shall pay all amounts that were withheld during the period of non-compliance, if the insured person provides a reasonable explanation for not submitting to the designated assessment or not complying with paragraph 2 or 4 of subsection (1), as the case may be. O. Reg. 281/03, s. 21.
(4) After conducting the designated assessment, the person or persons who conducted the designated assessment shall prepare a report and provide a copy of the report to,
(a) the insurer;
(b) the insured person; and
(c) the insured person’s health practitioner. O. Reg. 281/03, s. 21.
(5) Subject to subsection (11), the designated assessment centre shall deliver the report within 14 days after the completion of the designated assessment. O. Reg. 281/03, s. 21.
(6) If the designated assessment is required under section 37 in respect of a claim for an income replacement, non-earner or caregiver benefit, the report of the designated assessment shall include a statement as to whether the insured person continues to have a disability that entitles the insured person to continue to receive the benefit. O. Reg. 281/03, s. 21.
(7) If the designated assessment is required under section 37.2, the report of the designated assessment shall state whether the ancillary goods and services claimed in the treatment confirmation form are reasonable and necessary. O. Reg. 281/03, s. 21.
(8) If the designated assessment is required under section 38, the report of the designated assessment shall,
(a) state whether the goods or services to be provided under the treatment plan are reasonable and necessary and shall include recommendations relating to the future provision of goods and services to the insured person for his or her treatment and rehabilitation, if the purpose of the designated assessment is to determine if the goods and services are reasonable and necessary; and
(b) state whether the impairment comes within a Pre-approved Framework Guideline, if the purpose of the designated assessment is to determine if the insured person has an impairment to which a Pre-approved Framework Guideline applies. O. Reg. 281/03, s. 21.
(9) In the case of a designated assessment described in clause (8) (b), the report of the designated assessment centre shall also state whether the goods or services to be provided under the treatment plan are reasonable and necessary and shall include recommendations relating to the future provision of goods and services to the insured person for his or her treatment and rehabilitation, if the report states that the impairment does not come within a Pre-approved Framework Guideline. O. Reg. 281/03, s. 21.
(10) If the designated assessment is required under section 38.2, the report of the designated assessment shall state whether an expense in respect of an assessment or examination is payable under section 24. O. Reg. 281/03, s. 21.
(11) Despite subsection 53 (9), if the designated assessment is conducted to determine whether there are medical or rehabilitation benefits payable otherwise than under a Pre-approved Framework Guideline or the designated assessment is required under section 38.2, the designated assessment centre shall deliver its report to the insured person and the insurer within five business days after the later of,
(a) the day it receives the information required to be provided under paragraph 2 of subsection (1); or
(b) the day any conflict of interest disclosed by the designated assessment centre under section 53 in respect of the designated assessment is resolved under that section. O. Reg. 281/03, s. 21.
(12) If an insurer fails to give a notice required under subsection (1) in accordance with that subsection, the insurer shall pay for the goods and services that are the subject of the designated assessment and that relate to the period commencing on the day the insurer was required to give the notice and ending on the day the insurer gives the notice. O. Reg. 281/03, s. 21.
(13) If the designated assessment is required under section 39 in respect of a claim for an attendant care benefit, the report shall include,
(a) an assessment of attendant care needs in Form 1; and
(b) recommendations on the future provision of attendant care services to the insured person. O. Reg. 281/03, s. 21.
(14) If the designated assessment is required under section 40 to determine whether an impairment is a catastrophic impairment, the report shall include a statement of whether, in the opinion of the person or persons who conducted the designated assessment, the impairment is a catastrophic impairment. O. Reg. 281/03, s. 21.
44. (1) An insurer shall pay a benefit under this Regulation,
(a) by mailing or delivering a cheque payable to the person entitled to the benefit to the address where the person ordinarily resides; or
(b) with the consent of the person entitled to the benefit, by electronic funds transfer to an account in the name of the person.
(2) Despite subsection (1),
(a) an insurer may arrange to be invoiced directly and to pay directly for goods or services provided in respect of an insured person; or
(b) an insurer may pay a benefit into court under section 271 of the Insurance Act. O. Reg. 403/96, s. 44.
Explanation of Benefit Amounts
45. When a benefit is first paid or the amount of the benefit is subsequently changed, the insurer shall provide the insured person with a written explanation of how the amount of the benefit was determined. O. Reg. 403/96, s. 45.
46. (1) An amount payable in respect of a benefit is overdue if the insurer fails to pay the benefit within the time required under this Part.
(2) If payment of a benefit under this Regulation is overdue, the insurer shall pay interest on the overdue amount for each day the amount is overdue from the date the amount became overdue at the rate of 2 per cent per month compounded monthly. O. Reg. 403/96, s. 46.
47. (1) A person shall repay to the insurer,
(a) any benefit under this Regulation that is paid to the person as a result of an error on the part of the insurer, the insured person or any other person, or as a result of wilful misrepresentation or fraud;
(b) any income replacement or non-earner benefit that is paid to the person if he or she, or a person in respect of whom the payment was made, was disqualified from payment under Part IX;
(c) any income replacement, non-earner or caregiver benefit or any benefit under Part VI, to the extent of any payments received by the person that are deductible from those benefits under this Regulation;
(d) if subsection 37 (4) applies, any income replacement benefit, non-earner or caregiver benefit that is paid for the period after the insurer gives notice under subsection 37 (1) and before the date of the report of the designated assessment centre referred to in subsection 37 (4); or
(e) fees paid by the insurer under paragraph 2 of subsection 24 (1), if the insured person fails, without a reasonable explanation, to attend a designated assessment that has been arranged, or cancels a designated assessment without providing such notice as may be specified in the Pre-assessment Cancellation Fee Schedule established by the committee referred to in section 52, as it may be amended from time to time, that he or she will not be attending the designated assessment. O. Reg. 403/96, s. 47 (1); O. Reg. 281/03, s. 22.
(2) If a person is required to repay an amount to an insurer under this section,
(a) the insurer shall give the person notice of the amount that is required to be repaid; and
(b) if the person is receiving an income replacement or caregiver benefit, the insurer may give the person notice that the insurer intends to collect the repayment by deducting up to 20 per cent of the amount of the benefit from each payment of the benefit. O. Reg. 403/96, s. 47 (2).
(3) The obligation to repay a benefit does not apply unless the notice under subsection (2) is given within 12 months after the payment was made. O. Reg. 403/96, s. 47 (3).
(4) Subsection (3) does not apply if the benefit was paid as a result of wilful misrepresentation or fraud. O. Reg. 403/96, s. 47 (4).
(5) An insurer that has given the notice referred to in clause (2) (b) may collect the repayment by deducting up to 20 per cent of the amount of the benefit from each payment of the benefit. O. Reg. 403/96, s. 47 (5).
(6) The insurer may charge interest on an amount repayable under this section from the fifteenth day after notice is given under subsection (2) at the bank rate in effect on that day. O. Reg. 403/96, s. 47 (6).
(7) In subsection (6),
“bank rate” means the bank rate established by the Bank of Canada as the minimum rate at which the Bank of Canada makes short term advances to the banks listed in Schedule I to the Bank Act (Canada). O. Reg. 403/96, s. 47 (7).
Termination of Benefits for Material Misrepresentation
48. (1) If an insured person has wilfully misrepresented material facts with respect to an application for a benefit, the insurer may terminate payment of the benefit.
(2) The insurer shall not terminate payment under subsection (1) unless the insurer provides the insured person with notice of the reasons for terminating payment. O. Reg. 403/96, s. 48.
49. If an insurer refuses to pay a benefit under this Regulation or reduces the amount of a benefit that a person is receiving under this Regulation, the insurer shall provide the person with a written notice concerning the person’s right to dispute. O. Reg. 281/03, s. 23.
50. (1) An insured person shall not commence a mediation proceeding under section 280 of the Act unless,
(a) the insured person notified the insurer of the circumstances giving rise to a claim for a benefit and submitted an application for the benefit within the times prescribed by this Part;
(b) the insured person made himself or herself reasonably available for any examination required by the insurer under section 42, other than in relation to a medical or rehabilitation benefit under section 14 or 15; and
(c) the insured person has undergone any required designated assessment under section 43 and has complied with that section in respect of the designated assessment. O. Reg. 281/03, s. 24.
(2) Despite clause (1) (b), an insured person who does not attend an examination that has been scheduled shall not be considered to have made himself or herself reasonably available for the examination unless, before applying for mediation, the person attends a rescheduled appointment for the examination, if required by the insurer. O. Reg. 281/03, s. 24.
51. (1) A mediation proceeding or evaluation under section 280 or 280.1 of the Insurance Act or a court proceeding or arbitration under clause 281 (1) (a) or (b) of the Act in respect of a benefit under this Regulation shall be commenced within two years after the insurer’s refusal to pay the amount claimed.
(2) Despite subsection (1), a court proceeding or arbitration under clause 281 (1) (a) or (b) of the Insurance Act may be commenced within 90 days after the mediator reports to the parties under subsection 280 (8) of the Act or within 30 days after the person performing the evaluation provides a report to the parties under section 280.1 of the Act, whichever is later. O. Reg. 403/96, s. 51.
PART XI
DESIGNATED ASSESSMENT CENTRES
Establishment of Designated Assessment Centres
52. The committee appointed under section 7 of the Insurance Act shall,
(a) designate assessment centres for the purpose of this Regulation;
(b) specify the types of impairments that each designated assessment centre is authorized to assess; and
(c) specify the types of assessments that each designated assessment centre is authorized to conduct. O. Reg. 403/96, s. 52.
52.1 The committee referred to in section 52 may suspend, revoke or modify a designation under section 52, subject to such terms and conditions as the committee specifies. O. Reg. 281/03, s. 25.
52.2 (1) When required by the committee referred to in section 52, every designated assessment centre shall provide the Superintendent with such information respecting the performance of its functions as the committee may require. O. Reg. 281/03, s. 25.
(2) Information required under subsection (1) shall be provided at such times and in such manner as the committee may determine and direct. O. Reg. 281/03, s. 25.
(3) The Superintendent shall review the information compiled under subsection (1) and may take such action in respect of the information as the Superintendent considers appropriate. O. Reg. 281/03, s. 25.
(4) If a designated assessment centre fails to comply with a request for information under subsection (1), the Superintendent may report the deficiency to the committee referred to in section 52. O. Reg. 281/03, s. 25.
53. (1) A designated assessment shall be conducted by a designated assessment centre selected in accordance with this section. O. Reg. 313/03, s. 1 (1).
(1.1) A designated assessment must be conducted by a designated assessment centre that,
(a) is authorized to assess impairments of the type sustained by the insured person; and
(b) is authorized to conduct the type of designated assessment that is required. O. Reg. 313/03, s. 1 (1).
(1.2) A designated assessment must be conducted by a designated assessment centre that is located within,
(a) 30 kilometres of the insured person’s residence, if,
(i) the insured person’s residence is located in the City of Toronto or the regional municipality of Durham, Halton, Peel or York, and
(ii) a designated assessment centre that complies with subsection (1.1) is located within 30 kilometres of the insured person’s residence; or
(b) 50 kilometres of the insured person’s residence, if,
(i) the insured person’s residence is not located in the City of Toronto or the regional municipality of Durham, Halton, Peel or York, and
(ii) a designated assessment centre that complies with subsection (1.1) is located within 50 kilometres of the insured person’s residence. O. Reg. 313/03, s. 1 (1).
(1.3) Subject to subsections (1.1) and (1.2), the insurer and the insured person may jointly select the designated assessment centre if the selection is made not later than the second business day after the insurer or the insured person, as the case may be, receives notice from the other that a designated assessment is required under this Regulation. O. Reg. 313/03, s. 1 (1).
(1.4) If the insurer and the insured person do not jointly select the designated assessment centre in accordance with subsection (1.3), the Superintendent shall, subject to subsections (1.1) and (1.2), select the designated assessment centre. O. Reg. 313/03, s. 1 (1).
(2) If the designated assessment centre is selected by the Superintendent, the designated assessment centre shall, before conducting the designated assessment, give the insurer and the insured person notice disclosing any conflict of interest that the centre has relating to the designated assessment. O. Reg. 313/03, s. 1 (2).
(3) The designated assessment centre shall give any notice required under subsection (2) in respect of a designated assessment described in subsection 43 (11) within three business days after receipt of the request for the designated assessment. O. Reg. 281/03, s. 26.
(4) If a conflict of interest is disclosed under subsection (2),
(a) the designated assessment centre shall conduct the designated assessment if the insurer and the insured person agree; or
(b) if the insurer and the insured person do not agree, the designated assessment shall be conducted, subject to subsections (1.1), (1.2) and (2), by another designated assessment centre selected by the Superintendent. O. Reg. 281/03, s. 26; O. Reg. 313/03, s. 1 (3).
(5) For the purposes of clause (4) (b), the insurer and the insured person shall be deemed not to agree in the case of a designated assessment described in subsection 43 (11) unless they agree by the end of the third business day after the day the insurer receives the notice under subsection (2) or the insured person receives the notice under subsection (2), whichever day is later. O. Reg. 281/03, s. 26.
(6)-(8) Revoked: O. Reg. 313/03, s. 1 (4).
(9) Except as otherwise required under subsection 43 (11), a designated assessment centre must begin a designated assessment within 14 days after receiving a request for the designated assessment. O. Reg. 281/03, s. 26.
(10) If a designated assessment centre is unable to begin a designated assessment within 14 days after receiving the request for the assessment, the insured person or the insurer may require that, subject to subsections (1.1), (1.2) and (2), the designated assessment be conducted by another designated assessment centre selected by the Superintendent. O. Reg. 313/03, s. 1 (5).
(10.1) The Superintendent may, with the consent of the Minister, delegate in writing to any person the Superintendent’s authority to select designated assessment centres under this section. O. Reg. 313/03, s. 1 (5).
(11) For the purpose of this section, a designated assessment centre has a conflict of interest relating to a designated assessment if,
(a) the insurer, the insured person or a lawyer or other representative acting on behalf of the insurer or the insured person has a financial interest in the designated assessment centre; or
(b) the designated assessment centre, a related person, an assessor or consultant who will carry out all or part of the designated assessment or a facility owned or controlled, directly or indirectly, in whole or in part, by the centre or a related person,
(i) has provided goods or services to the person to be assessed, other than a previous designated assessment,
(ii) prepared or approved a treatment confirmation form under section 37.1, a treatment plan under section 38 or an application for approval of an assessment or examination under section 38.2 for the person to be assessed, or
(iii) is identified by a treatment confirmation form, treatment plan or an application for approval of an assessment or examination as a person who will provide goods or services to the person to be assessed. O. Reg. 281/03, s. 26.
(12) In clause (11) (b),
“related person” means, in respect of a designated assessment centre, an owner, partner or another person who has a financial interest in the designated assessment centre, but does not include a person who has a financial interest in the designated assessment centre by reason only of being a creditor who deals at arm’s length with the designated assessment centre. O. Reg. 281/03, s. 26.
54. (1) A designated assessment centre that conducts an assessment under this Regulation of a person who sustains an impairment as a result of an accident shall not, after the assessment, provide any goods or services to the person in respect of the accident.
(2) Subsection (1) does not apply if,
(a) the insured person and the insurer agree; or
(b) there is no other person within 50 kilometres of the insured person’s residence who is able to provide the goods or services.
(3) Subsection (1) does not prevent the designated assessment centre from conducting another assessment of the person. O. Reg. 403/96, s. 54.
PART XII
RESPONSIBILITY TO OBTAIN TREATMENT, PARTICIPATE IN REHABILITATION AND SEEK EMPLOYMENT
55. (1) An insured person entitled to an income replacement, non-earner or caregiver benefit shall obtain such treatment and participate in such rehabilitation as is reasonable, available and necessary to,
(a) permit the insured person to engage in employment that satisfies the criteria set out in subsection (2), in the case of an insured person entitled to an income replacement benefit; or
(b) shorten the period during which the benefit is payable, in any other case. O. Reg. 403/96, s. 55 (1).
(2) The criteria referred to in clause (1) (a) are:
1. The insured person,
i. is able and qualified to perform the essential tasks of the employment, or
ii. would be able and qualified to perform the essential tasks of the employment if the insured person obtained treatment and participated in rehabilitation that is reasonable, available and necessary to permit the person to engage in the employment.
2. The employment exists in the area in which the insured person lives.
3. It would be reasonable to expect the insured person to engage in the employment having regard to the possibility of deterioration in the insured person’s impairment and to the insured person’s personal and vocational characteristics. O. Reg. 403/96, s. 55 (2).
(3) Subsection (1) does not apply if compliance with subsection (1) would be detrimental to the insured person’s treatment or recovery. O. Reg. 403/96, s. 55 (3).
(4) If an insured person does not comply with subsection (1), the insurer may notify the insured person that the insurer intends to stop payment of the benefit in accordance with subsection (5). O. Reg. 281/03, s. 28.
(5) If at least 14 days have elapsed after a notice was given under subsection (4) and the insured person has not complied with subsection (1), the insurer may stop payment of the benefit. O. Reg. 281/03, s. 28.
(6) Section 37 does not apply in respect of a stoppage of benefits, or proposed stoppage of benefits, under this section. O. Reg. 281/03, s. 28.
(7) If, after the stoppage of benefits under subsection (5), the insured person subsequently complies with subsection (1), the insurer shall resume payment of the benefit in respect of periods after the insured person complied. O. Reg. 281/03, s. 28.
56. (1) An insured person who is entitled to an income replacement benefit shall make reasonable efforts to,
(a) return to the employment in which he or she engaged at the time of the accident; or
(b) obtain employment for which he or she is reasonably suited by education, training or experience. O. Reg. 403/96, s. 56 (1).
(2) Subsection (1) does not apply if,
(a) employment would be detrimental to the insured person’s treatment or recovery; or
(b) the insured person is participating in a vocational rehabilitation program. O. Reg. 403/96, s. 56 (2).
(3) If an insured person does not comply with subsection (1), the insurer may notify the insured person that the insurer intends to stop payment of the benefit in accordance with subsection (4). O. Reg. 281/03, s. 29.
(4) If at least 14 days have elapsed after a notice is given under subsection (3) and the insured person is not in compliance with subsection (1), the insurer may stop payment of the benefit. O. Reg. 281/03, s. 29.
(5) Section 37 does not apply in respect of a stoppage of benefits, or proposed stoppage of benefits, under this section. O. Reg. 281/03, s. 29.
(6) If, after the stoppage of benefits under subsection (4), the insured person subsequently complies with subsection (1), the insurer shall resume payment of the benefit in respect of periods after the insured person complied. O. Reg. 281/03, s. 29.
PART XIII
INTERACTION WITH OTHER SYSTEMS
57. (1) If, as a result of an accident in another province or territory of Canada or a jurisdiction in the United States of America, a person insured in that jurisdiction dies or sustains an impairment or incurs an expense described in section 14, 15 or 16, the insurer shall pay, as the person may elect,
(a) benefits provided by this Regulation, other than the benefits referred to in clause (b); or
(b) benefits in the same amounts and subject to the same conditions as if the person was a resident of the jurisdiction in which the accident occurred and was entitled to payments under the law of that jurisdiction. O. Reg. 403/96, s. 57 (1).
(1.1) Subsection (1) does not apply if the person receives benefits under the law of the jurisdiction in which the accident occurred. O. Reg. 462/96, s. 8 (1).
(2) A person who elects to claim a benefit as provided in clause (1) (a) is thereafter eligible only for benefits referred to in that clause. O. Reg. 403/96, s. 57 (2).
(3) A person who elects to claim a benefit as provided in clause (1) (b) is thereafter ineligible for benefits referred to in clause (1) (a). O. Reg. 403/96, s. 57 (3).
(4) For the purpose of this section, a person is insured in the jurisdiction in which the accident occurred if the person, at the time of the accident,
(a) was authorized by law to be or to remain in Canada and was living and ordinarily present in Ontario;
(b) met the criteria prescribed for recovery under the law of the jurisdiction in which the accident occurred;
(c) was not the owner or driver of, or an occupant of an automobile registered in the jurisdiction in which the accident occurred; and
(d) was,
(i) an occupant of the insured automobile,
(ii) the named insured, a person specified in the policy as a driver of the insured automobile, the spouse of the named insured or a dependant of the named insured or spouse, while the occupant of any automobile,
(iii) a person who was not the occupant of an automobile and was struck by the insured automobile,
(iv) the named insured, his or her spouse or a dependant of the named insured or spouse and was struck by any automobile,
(v) if the named insured is a corporation, unincorporated association, partnership or sole proprietorship, a person for whose regular use the insured automobile was supplied, his or her spouse or a dependant of the person or spouse who suffered an impairment,
(A) while the occupant of any automobile,
(B) by any automobile while not the occupant of the automobile, or
(vi) a person struck by an automobile that was driven by a person described in subclause (i), (ii) or (v). O. Reg. 403/96, s. 57 (4); O. Reg. 462/96, s. 8 (2); O. Reg. 114/00, s. 6; O. Reg. 314/05, s. 6.
58. (1) The insurer shall pay benefits under this Regulation even though the insured person is entitled to, or has received, benefits under an Act administered by the Ministry of Community and Social Services for Ontario or under similar legislation in another jurisdiction.
(2) For the purpose of subsection (1), a service, benefit or entitlement provided under an Act, the administration of which was transferred from the Ministry of Community and Social Services to the Ministry of Health by order in council, shall be deemed to be provided under an Act administered by the Ministry of Community and Social Services for Ontario so long as the nature of the service, benefit or entitlement remains substantially the same as it was before the transfer. O. Reg. 403/96, s. 58.
Workers’ Compensation Benefits
59. (1) The insurer is not required to pay benefits under this Regulation in respect of any insured person who, as a result of an accident, is entitled to receive benefits under any workers’ compensation law or plan. O. Reg. 403/96, s. 59 (1).
(2) Subsection (1) does not apply in respect of an insured person who elects to bring an action referred to in section 30 of the Workplace Safety and Insurance Act, 1997 so long as the election is not made primarily for the purpose of claiming benefits under this Regulation. O. Reg. 403/96, s. 59 (2); O. Reg. 281/03, s. 30 (1).
(3) If a person is entitled to receive benefits under this Regulation as a result of an election made under section 30 of the Workplace Safety and Insurance Act, 1997, no income replacement, caregiver or non-earner benefit is payable to the person in respect of any period of time before the person makes the election. O. Reg. 403/96, s. 59 (3); O. Reg. 462/96, s. 9; O. Reg. 281/03, s. 30 (2).
(4) If a person who would be entitled to benefits under this Regulation in the absence of subsection (1) elects to bring an action referred to in section 30 of the Workplace Safety and Insurance Act, 1997 and there is a dispute concerning the insurer’s liability to pay an expense for a vocational rehabilitation program that the person was attending at the time of the election and continues to attend, the insurer shall pay the expense pending resolution of the dispute. O. Reg. 403/96, s. 59 (4); O. Reg. 281/03, s. 30 (3).
(5) Despite subsection (1), if there is a dispute about whether subsection (1) applies to a person, the insurer shall pay full benefits to the person under this Regulation pending resolution of the dispute if,
(a) the person makes an assignment to the insurer of any benefits under any workers’ compensation law or plan to which he or she is or may become entitled as a result of the accident; and
(b) the administrator or board responsible for the administration of the workers’ compensation law or plan approves the assignment. O. Reg. 403/96, s. 59 (5).
60. (1) The insurer may deduct the following amounts from the amount payable to an insured person as an income replacement or non-earner benefit:
1. Any temporary disability benefits being received by the insured person in respect of a period following the accident and in respect of an impairment that occurred before the accident.
2. Any other periodic benefit being received by the insured person in respect of a period following the accident and in respect of an impairment that occurred before the accident, if the insured person was receiving the other periodic benefit at the time he or she first qualified for the income replacement or non-earner benefit, and, at that time, the other periodic benefit was a temporary disability benefit. O. Reg. 403/96, s. 60 (1).
(2) Payment of a medical, rehabilitation or attendant care benefit or a benefit under Part VI is not required for that portion of an expense for which payment is reasonably available to the insured person under any insurance plan or law or under any other plan or law. O. Reg. 403/96, s. 60 (2).
(3) In this section,
“temporary disability benefit” means,
(a) an income replacement or non-earner benefit paid under this Regulation, unless the benefit is paid more than 104 weeks after the onset of the disability,
(b) a caregiver benefit paid under this Regulation,
(c) benefits paid under Part II, III or IV or section 32 of Ontario Regulation 776/93,
(d) benefits paid under Part V of Ontario Regulation 776/93, unless the benefits have been paid for more than 104 weeks,
(e) benefits paid under Part IV of Regulation 672 of the Revised Regulations of Ontario, 1990, unless the benefits have been paid for more than 156 weeks,
(f) benefits paid under Part II of Subsection 2 of Schedule C to the Insurance Act as it existed before June 22, 1990, unless the benefits have been paid for more than 104 weeks,
(g) benefits paid under section 37, subsection 43 (9) or subsection 147 (2) of the pre-1997 Act, as defined in Part IX of the Workplace Safety and Insurance Act, 1997, in respect of injuries that occurred before January 1, 1998, including benefits paid under those provisions as those provisions are deemed to have been amended by Part IX of the Workplace Safety and Insurance Act, 1997,
(g.1) benefits paid under subsection 43 (3) of the Workplace Safety and Insurance Act, 1997 in respect of injuries that occurred after December 31, 1997, or
(h) any other periodic temporary benefit paid under an income continuation benefit plan or law, other than,
(i) benefits under the Employment Insurance Act (Canada),
(ii) a non-earner benefit paid under this Regulation more than 104 weeks after the onset of the disability,
(iii) benefits paid under Part V of Ontario Regulation 776/93 for more than 104 weeks,
(iv) benefits paid under Part IV of Regulation 672 of the Revised Regulations of Ontario, 1990 for more than 156 weeks, or
(v) benefits paid under Part II of Subsection 2 of Schedule C to the Insurance Act as it existed before June 22, 1990 that have been paid for more than 104 weeks. O. Reg. 403/96, s. 60 (3); O. Reg. 462/96, s. 10; O. Reg. 281/03, s. 31.
61. (1) For the purpose of this Regulation, a person’s net weekly income from employment shall be determined in accordance with the following formula:
A = (B – C – D – E)/52
where,
A = the person’s net weekly income from employment,
B = the person’s gross annual income from employment,
C = the annual premium payable by the person under the Employment Insurance Act (Canada) on the gross annual income from employment,
D = the annual contribution payable by the person under the Canada Pension Plan on the gross annual income from employment,
E = the income tax payable by the person under the Income Tax Act (Canada) and the Income Tax Act (Ontario) on the gross annual income from employment.
(2) For the purpose of subsection (1), the person whose net weekly income from employment is to be determined shall be deemed to be a resident of Ontario. O. Reg. 403/96, s. 61.
62. (1) For the purpose of this Regulation, a person’s income from self-employment shall be determined in the same manner as the person’s profit from the business in which the person was self-employed would be determined under the Income Tax Act (Canada) and the Income Tax Act (Ontario), but without taking into account,
(a) expenses that are eligible for capital cost allowance or an allowance on eligible capital property;
(b) capital gains or losses; or
(c) losses deductible under section 111 of the Income Tax Act (Canada).
(2) Despite subsection (1), an insurer and a named insured who is self-employed and not otherwise employed may agree in a contract evidenced by a motor vehicle liability policy that, for the purpose of determining benefits under this Regulation in respect of an accident that occurs during the period covered by the contract, the named insured’s gross income from self-employment for every week shall be deemed to be the weekly income amount specified in the contract if, at the time of the accident, the person continues to engage in the self-employment in which he or she engaged at the time the contract was entered into and the person is not otherwise employed.
(3) In specifying a weekly income amount for the purpose of subsection (2), the insurer and insured may use information from any source, including,
(a) personal and corporate income tax returns and assessments;
(b) personal and corporate financial statements; and
(c) published data on the average wage for the industry or occupation in which the insured is self-employed. O. Reg. 403/96, s. 62.
63. (1) For the purpose of this Regulation, the income tax payable by a person under the Income Tax Act (Canada) and the Income Tax Act (Ontario) shall be determined having regard to only the following deductions and tax credits that apply to the person under those Acts:
1. Alimony and maintenance payments deduction.
2. Basic personal tax credit.
3. Married person’s tax credit or equivalent to married tax credit.
4. Age tax credit.
5. Disability tax credit.
6. Employment insurance premium tax credit.
7. Canada Pension Plan tax credit.
8. Quebec Pension Plan tax credit. O. Reg. 403/96, s. 63 (1).
(2) If a determination of the income tax payable by a person under the Income Tax Act (Canada) and the Income Tax Act (Ontario) is necessary to determine the amount of a benefit under this Regulation, the applicant for the benefit shall provide the insurer with such information as is reasonably necessary to enable the insurer to make the determination. O. Reg. 462/96, s. 11.
(3) Failure to comply with subsection (2) does not relieve the insurer from any time limit established by this Regulation for the payment of the benefit, but the insurer shall determine the amount of the benefit on the basis of its best estimate of the income tax payable by the person under the Income Tax Act (Canada) and the Income Tax Act (Ontario), subject to later adjustment of the amount of the benefit when subsection (2) is complied with. O. Reg. 403/96, s. 63 (3).
64. For the purpose of this Regulation, payments of severance pay or termination pay shall not be included in a determination of a person’s income. O. Reg. 403/96, s. 64.
64.1 (1) If, under the Income Tax Act (Canada) or legislation of another jurisdiction that imposes a tax calculated by reference to income, a person is required to report the amount of his or her income, the person’s income before an accident that occurs after April 14, 2004 shall be determined for the purposes of this Regulation without reference to any income the person has failed to report contrary to that Act or legislation. O. Reg. 458/03, s. 11.
(2) Where the amount of a person’s income before an accident is determined for the purposes of this Regulation in accordance with subsection (1), the amount of the income may be adjusted to reflect any change in the amount of the person’s income reported or determined in accordance with the Income Tax Act (Canada) or legislation of another jurisdiction that imposes a tax calculated by reference to income. O. Reg. 458/03, s. 11.
65. (1) The assignment of a benefit under this Regulation, or the assignment of the right to pursue a mediation, arbitration, appeal or variation proceeding under sections 280 to 284 of the Act, is void. O. Reg. 281/03, s. 32 (1).
(2) Subsection (1) does not apply to,
(a) an assignment under section 267.8 of the Insurance Act;
(b) an assignment of a benefit to,
(i) the Ministry of Community, Family and Children’s Services,
(ii) a delivery agent under the Ontario Disability Support Program Act, 1997 or the Ontario Works Act, 1997, or
(iii) The Minister of Finance under subsection 6.1 (4) of the Motor Vehicle Accident Claims Act; or
(c) the assignment of a benefit to the Ministry of Health in respect of a service, benefit or entitlement provided under an Act the administration of which was transferred by order in council from the Ministry of Community and Social Services to the Ministry of Health. O. Reg. 403/96, s. 65 (2); O. Reg. 281/03, s. 32.
Company Automobiles and Rental Automobiles
66. (1) An individual who is living and ordinarily present in Ontario shall be deemed for the purpose of this Regulation to be the named insured under the policy insuring an automobile at the time of an accident if, at the time of the accident,
(a) the insured automobile is being made available for the individual’s regular use by a corporation, unincorporated association, partnership, sole proprietorship or other entity; or
(b) the insured automobile is being rented by the individual for a period of more than 30 days. O. Reg. 403/96, s. 66 (1); O. Reg. 462/96, s. 12 (1).
(2) An individual who is not living and ordinarily present in Ontario shall be deemed for the purpose of this Regulation to be the named insured under the policy insuring an automobile at the time of an accident if, at the time of the accident,
(a) the insured automobile is being made available for the individual’s regular use by a corporation, unincorporated association, partnership, sole proprietorship or other entity; and
(b) the individual, his or her spouse or any dependant of the individual or spouse is an occupant of the insured automobile. O. Reg. 403/96, s. 66 (2); O. Reg. 462/96, s. 12 (2); O. Reg. 114/00, s. 7; O. Reg. 314/05, s. 7.
67. On request, the insurer shall provide a copy of this Regulation without charge to a named insured or a person entitled to benefits under this Regulation. O. Reg. 403/96, s. 67.
68. (1) All notices required or permitted under this Regulation, other than a notice under subsection 24 (1.3), 32 (1) or (3.1) or paragraph 3 of subsection 43 (1), shall be in writing. O. Reg. 281/03, s. 33.
(2) Any document, including a notice in writing, required or permitted under this Regulation to be given to a person may be delivered,
(a) by faxing the document to the person or to the solicitor or authorized representative, if any, of the person in accordance with subsection (6);
(b) by leaving a copy of the document with the solicitor or authorized representative, if any, of the person, or with an employee in the office of the solicitor or authorized representative;
(c) by personal delivery to the person; or
(d) by letter mail, certified mail or registered mail,
(i) in the case of an insurer, addressed to the insurer or its chief executive officer at the insurer’s head office in Ontario as identified in the records of the Superintendent, or
(ii) in the case of a person other than an insurer, addressed to the person at his or her last known address. O. Reg. 281/03, s. 33.
(3) Despite clause (2) (d), any notice or other document that must be given within five or fewer business days shall not be delivered by letter mail. O. Reg. 281/03, s. 33; O. Reg. 458/03, s. 12.
(4) If an attempt is made to personally deliver a document to a person at his or her place of residence and, for any reason, it is not possible to personally deliver the document to the person, the document may be delivered by leaving a copy, in a sealed envelope addressed to the person, at the person’s place of residence with anyone who appears to be an adult member of the same household. O. Reg. 380/03, s. 3.
(5) In the absence of evidence to the contrary, a person is deemed to receive anything delivered by letter mail under clause (2) (d) on the fifth business day after the day the document is mailed in accordance with clause (2) (d). O. Reg. 380/03, s. 3; O. Reg. 458/03, s. 12.
(6) A document that is delivered by fax must include a cover page indicating,
(a) the sender’s name, address and telephone number;
(b) the name of the person for whom the document is intended;
(c) the date of the accident to which the document relates;
(d) the name, address and telephone number of the person to whom the document relates;
(e) the date and time the fax is sent;
(f) the total number of pages faxed, including the cover page;
(g) the telephone number from which the document is faxed; and
(h) the name and telephone number of a person to contact in the event of transmission problems with the fax. O. Reg. 281/03, s. 33.
(7) A document delivered in accordance with clause (2) (a), (b) or (c) after 5 p.m. local time of the recipient shall be deemed to be delivered on the next business day. O. Reg. 281/03, s. 33.
(8) Despite subclause (2) (d) (i) and subsections (5) and (7), if the insurer provides the name and address of a contact person to whom documents are to be delivered, anything delivered to the insurer that is not addressed to the attention of the contact person at that address shall not be considered to have been delivered to the insurer until it is received by the contact person. O. Reg. 281/03, s. 33.
(9) A reference in this Regulation to a number of days between two events shall be read as excluding the day on which the first event happens and including the day on which the second event happens. O. Reg. 281/03, s. 33.
(10) Subject to subsection (11), if any provision of this Regulation requires a person to do anything within a time period expressed in days or business days, the time period is deemed to expire on the last day of the time period at 5 p.m. local time. O. Reg. 281/03, s. 33.
(11) If a time period in which a person is required to do anything expires on a day that is not a business day, the time period is deemed to expire on the next day that is a business day at 5 p.m. local time. O. Reg. 281/03, s. 33.
(12) For the purposes of subsections (10) and (11), if the person delivering a document or notice and the person to whom the document or notice is to be delivered are in different time zones, references to 5 p.m. local time shall be read as references to the time when it is 5 p.m. in one time zone and after 5 p.m. in the other time zone. O. Reg. 281/03, s. 33.
69. Each of the following documents shall be in a form approved by the Superintendent:
1. An application form referred to in clause 32 (2) (a).
2. A certificate required under section 34.
3. A notice under section 36.
4. A notice under subsection 37 (1).
5. A treatment confirmation form under section 37.1.
6. An application referred to in section 38, including the treatment plan.
7. An application under section 38.2.
8. An application under subsection 40 (1).
9. A notice under subsection 40 (2).
10. A report of a designated assessment.
11. An explanation under section 45.
12. A notice under section 49. O. Reg. 281/03, s. 34.
70. (1) Despite anything else in this Regulation, if a motor vehicle liability policy is in effect on the day this Regulation comes into force, subsections (2) and (3) apply until the earlier of the following:
1. The first expiry date under the motor vehicle liability policy.
2. The date on which the motor vehicle liability policy is terminated by the insurer or the insured.
(2) The following benefits are deemed to be included in the motor vehicle liability policy, and are applicable to an insured person in respect of the motor vehicle liability policy:
1. The optional income replacement benefit referred to in paragraph 1 of subsection 27 (1) that fixes the amount referred to in subparagraph ii of paragraph 2 of subsection 7 (1) at $1,000.
2. The optional caregiver and dependant care benefit referred to in paragraph 2 of subsection 27 (1).
3. The optional death and funeral benefit referred to in paragraph 4 of subsection 27 (1).
(3) The sum of the medical, rehabilitation and attendant care benefits paid under the motor vehicle liability policy for any one accident in respect of an insured person who does not sustain a catastrophic impairment as a result of the accident shall not exceed $1,000,000, and the limits set out in clauses 19 (1) (a) and (2) (a) do not apply. O. Reg. 403/96, s. 70.
70.1 Form 1, as it read on September 30, 2003, continues to apply in respect of accidents occurring before October 1, 2003. O. Reg. 281/03, s. 35.
71. Omitted (provides for coming into force of provisions of this Regulation). O. Reg. 403/96, s. 71.
Form 1
assessment of attendant care needs
Insurance Act
Insert regs\graphics\1996\403\403001ae.tif
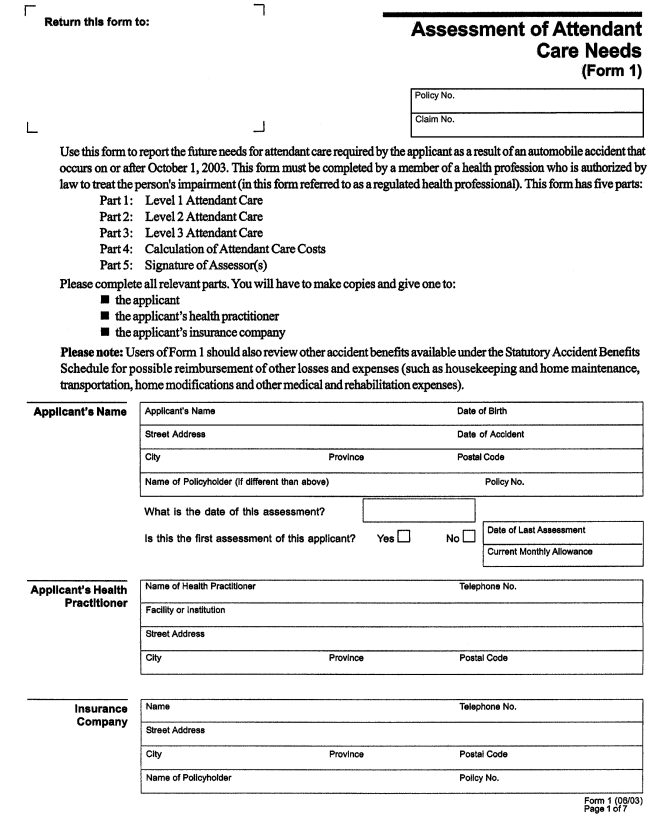
Insert regs\graphics\1996\403\403001be.tif
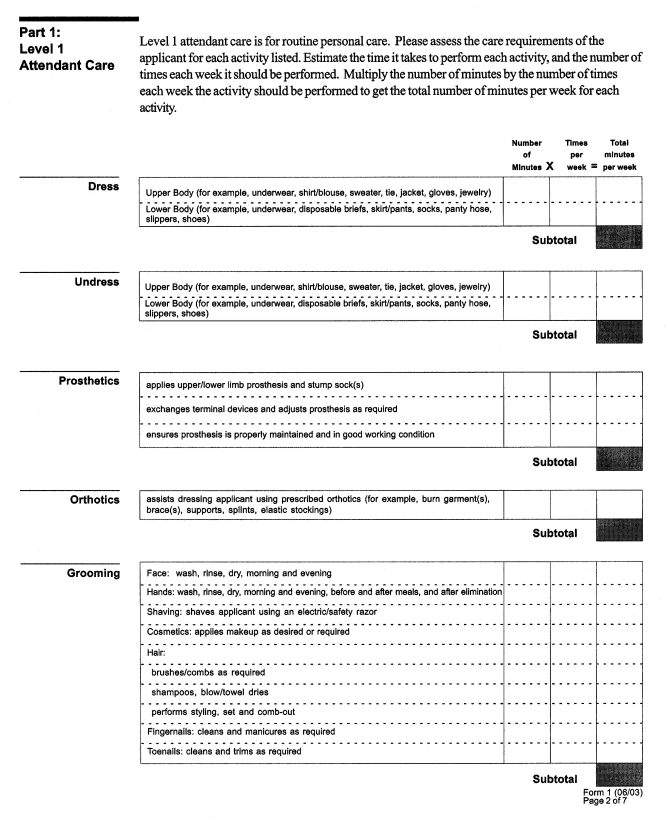
Insert regs\graphics\1996\403\403001ce.tif
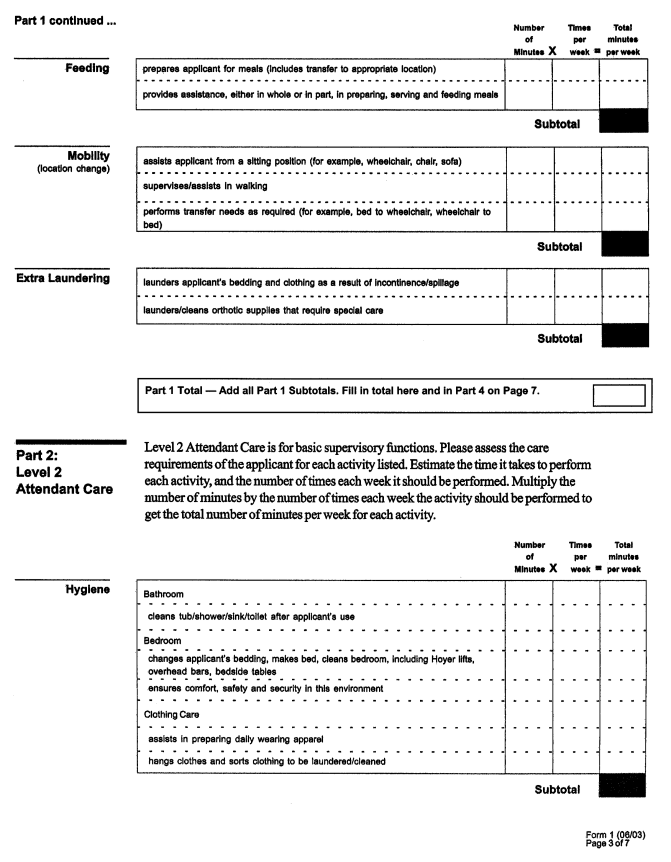
Insert regs\graphics\1996\403\403001de.tif
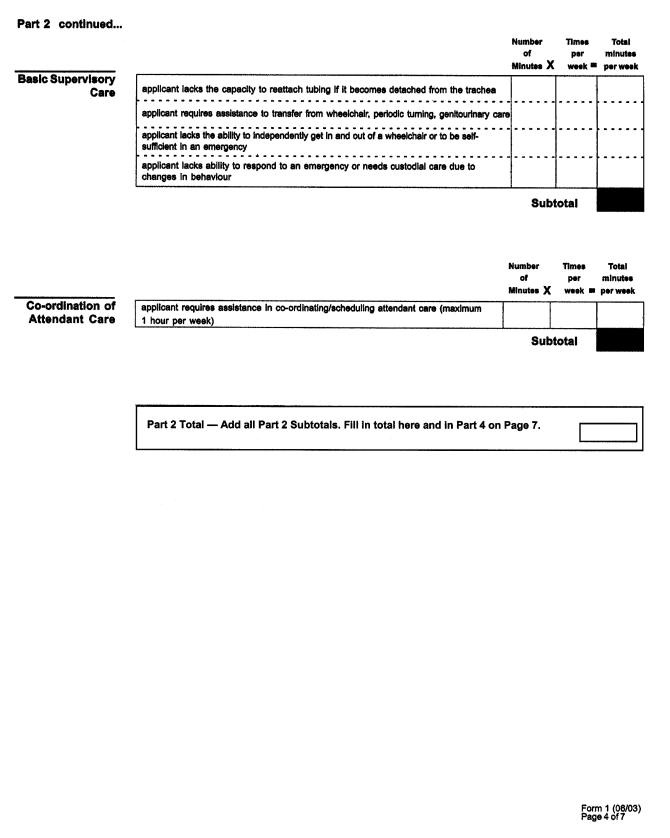
Insert regs\graphics\1996\403\403001ee.tif
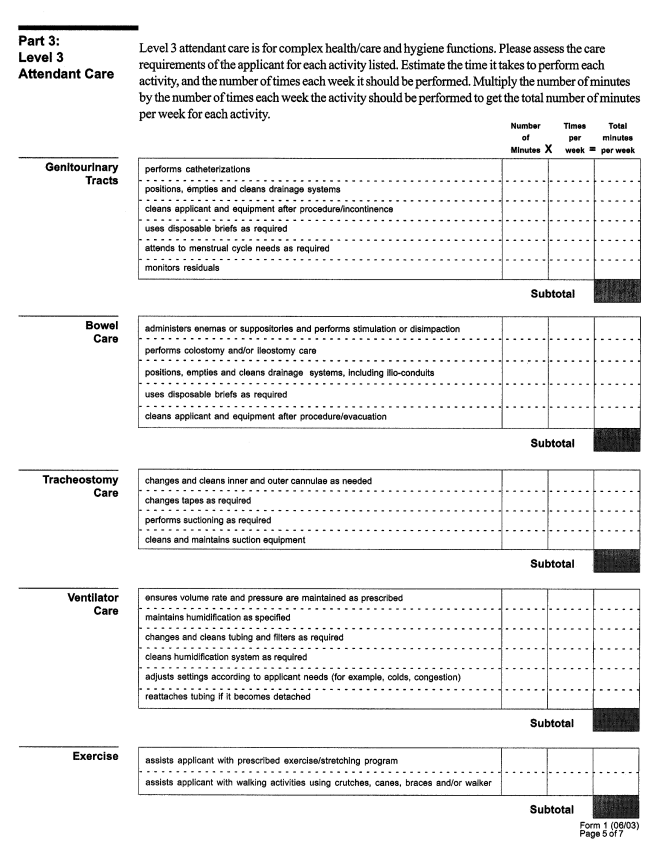
Insert regs\graphics\1996\403\403001fe.tif
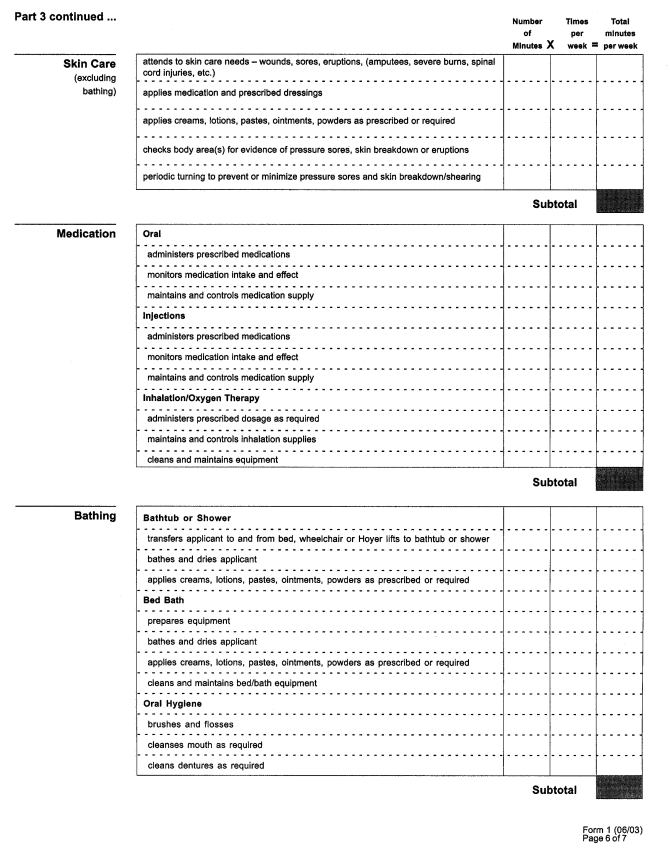
Insert regs\graphics\1996\403\403001ge.tif
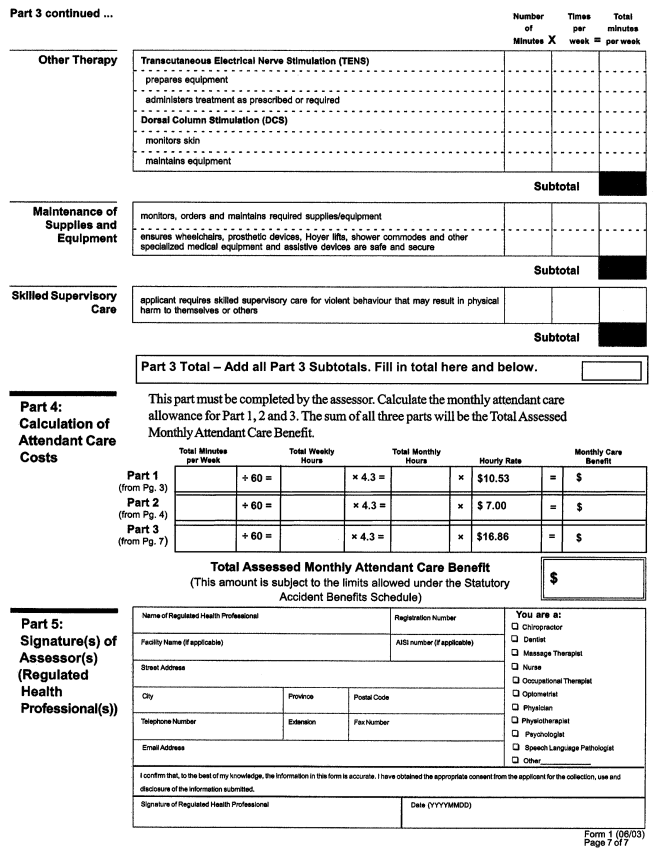
O. Reg. 281/03, s. 36.