A better place to live, a better place to work: Ontario’s long-term care staffing plan
We are making long-term care a better place for residents to live, and a better place for staff to work. Read our plan to recruit and retain more staff, improve working conditions, and drive effective and accountable leadership.
Minister’s message
As we launch this historic staffing plan in December 2020, it is clear, now more than ever, that immediate and deliberate action is needed to improve Ontario’s long-term care sector so that we can protect, provide appropriate care and bring dignity to our most vulnerable today and into the future.
These have been challenging times, as the COVID-19 pandemic revealed the weaknesses and inadequacies within the long-term care system. These are issues that had been developing over decades of neglect and underfunding.
To those working in our long-term care homes, I would like to express my sincere gratitude. You are the frontline health care heroes who work tirelessly every day to support our loved ones. Our government knows that staff in long-term care homes are the backbone of the sector. Nurses, personal support workers, allied health professionals and support staff all play a vital role in the quality of life that residents experience.
Since our government created a stand-alone Ministry of Long-Term Care in 2019, we have worked diligently to ensure that our most vulnerable have access to the care they deserve, when and where they need it. This is at the centre of everything we do.
While we have already begun to make real progress in creating a 21st century long-term care sector that is resident-centred, we know it is critical that we address the long-standing and systemic staffing challenges the sector has faced.
In our 2020 Budget, we committed to increasing the hours of direct care for long-term care residents to an average of four hours per day, making Ontario the Canadian leader in the provision of care. To achieve this new standard, based on guidance from multiple partners, organizations, associations, residents and families, the Staffing Study Advisory Group, and the Long-Term Care COVID-19 Commission, we are launching A better place to live, a better place to work: Ontario’s long-term care staffing plan.
I want to extend my sincere thanks to all sector partners who have helped develop this plan. It will take concerted effort, significant new investment and sustained collaboration to drive change.
Having worked as a family physician for almost three decades, and as a daughter who had a parent in long-term care, I deeply appreciate the difficult and rewarding work that frontline health care staff provide. I want to thank every single one of you for your commitment to making long-term care a place where our loved ones are safe and cared for. For those of you considering a career in long-term care, welcome, we need you, our most vulnerable need you.
Sincerely,
Dr. Merrilee Fullerton
Minister of Long-Term Care
Executive summary
As part of our aggressive modernization plan, the government has taken steps to create a long-term care sector that is resident-centered and provides the highest quality of care for our loved ones, when and where they need it. This includes a commitment to invest $1.75 billion to create 30,000 modern long-term care spaces over ten years.
As the government builds capacity, it is critical that staffing challenges are addressed in Ontario’s long-term care sector. The recommendations in the Long-Term Care Staffing Study released in July 2020, which were further confirmed through the interim recommendations from Ontario’s Long-Term Care COVID-19 Commission, strongly suggest that the conditions of work for staff are closely tied to the conditions of care for residents.
The devastating impact of the COVID-19 pandemic on the long-term care sector further shone a light on the complexity of the staffing challenges in the sector. The government has invested over half a billion dollars to prevent and contain viral spread during the second wave, including educating, recruiting and retaining over 3,700 more health care workers.
While these actions are critical to address urgent staff shortages and support long-term care homes through the COVID-19 pandemic, addressing the long-standing and systemic staffing issues will take concerted effort, significant new investment and sustained collaboration with all sector partners to drive change. That is why the province is launching A better place to live, a better place to work: Ontario’s long-term care staffing plan, based on guidance from multiple partners, organizations, associations, residents and families, the Staffing Study Advisory Group and the interim recommendations from Ontario’s COVID-19 Commission.
At the centre of this plan is the government’s commitment to increase the hours of direct care for residents to an average of four hours per day over four years. This will require the education and training of new professionals to fill the more than 27,00 full-time equivalent jobs which will be needed to reach this standard. To implement this plan, the government will be investing up to $1.9 billion annually by 2024–2025.
The vision of the plan is to enable a qualified and engaged workforce—working with effective and accountable leadership—to provide residents with a safe and supportive living environment. The plan focuses on six key areas of action:
- Increasing staffing levels
- Increase the average amount of direct hands-on care provided by registered nurses, registered practical nurses and personal support workers to four hours a day per resident, with an increased focus on nursing care.
- An additional, per resident increase in the amount of allied health support provided by others such as physiotherapists, occupational therapists and social workers.
- Issue guidance on staffing models to long-term care homes.
- Disrupting, accelerating and increasing education and training pathways
- Stabilize staffing through initiatives to recruit, retain, train and support more staff, such as the Ontario Matching Portal, increased infection prevention and control personnel, Personal Support Worker Return of Service program, fast tracking personal support worker (PSW) education, providing supports for new nursing graduates and the Ontario Workforce Reserve for Senior Support Program.
- Accelerate and create new pathways to increase supply of workers. Immediate focus includes removing barriers to employment for internationally educated professionals, training personal support workers on the job and supporting career laddering, including PSWs who want to become registered practical nurses and registered practical nurses who want to become registered nurses.
- Scale up traditional education and training streams to create new labour supply in partnership with educational institutions.
- Launch targeted awareness and recruitment campaigns to drive enrollment and employment.
- Supporting ongoing staff development
- Provide enhanced Infection Prevention and Control Education and Training for new and existing staff.
- Invest $10 million in an annual training fund to support staff education.
- Work with the sector to develop and implement initiatives that support career growth and satisfaction, such as mentorships, preceptorships and communities of practice.
- Improving working conditions
- Partner with sector leaders to drive improvements to working conditions, including increased full-time employment.
- Reduce administrative burden by reviewing components of the province’s funding formula for long-term care, including documentation and reporting requirements where they are unnecessary for resident care and resident outcomes.
- Promote innovative approaches to work and technology.
- Providing effective and accountable leadership
- Increase the number of Attending Nurse Practitioners in long-term care and conduct an assessment of further needs.
- Support Medical Directors as they navigate their work and clarify the expectations, accountabilities and requirements of the role.
- Promote leadership onboarding and training.
- Support development and education of home administrators.
- Measuring success
- Enhance data collection to gather the necessary information to accurately measure plan’s success.
- Measure the plan’s success against targets and indicators.
- Evaluate success and report publicly.
Overcoming the current, long-standing challenges in long-term care will require a sustained effort over the years ahead and close collaboration of all partners. Working together, this vision for long-term care residents can be a reality, ensuring that long-term care homes are a better place to live, and a better place to work.
Introduction
Context for change
The long-term care system exists to support Ontarians with advanced care needs, who require frequent assistance with activities of daily living, and on-site care and medical supervision that can no longer be provided in their own homes.
The staffing challenges facing Ontario’s long-term care sector are well documented. Ontario’s population is aging, and there is increasing demand for long-term care beds. As well, the medical complexity of residents has increased by more than 15% over the past 15 years, requiring increasingly more qualified staff to provide appropriate care.
From the many reports, submissions and recommendations this government has received, the messaging has been consistent: more staff and better working conditions are critical to ensure residents receive quality care.
The Long-Term Care Staffing Study Advisory Group engaged with over 25 organizations representing care providers, residents and family, operators, nursing organizations, labour unions and training and research.
The Long-Term Care Staffing Plan is informed by reports and submissions from these organizations and additional long-term care partners, and by the formal recommendations outlined in the following reports:
- long-term care homes public inquiry
- long-term care staffing study
- long-term care COVID-19 commission interim recommendations
Detail on how the staffing plan responds to specific recommendations is described in the pages that follow.
Considerable staff recruitment and retention efforts will be required to achieve the goals of the plan. In addition, the government has committed to expanding long-term care capacity by building 30,000 spaces in the long-term care sector to address wait times and preparing for future demand. Thousands of new, qualified staff are required to support this increased capacity.
A resident-centred long-term care sector
Long-term care provides a home for some of our province’s most vulnerable residents. The province has taken steps to create a modernized sector where care needs are consistently met, residents enjoy a good quality of life and the public has confidence knowing that their loved ones will have a safe place to call home. The government is taking action in four pillars to reach these outcomes:
- integrating long-term care within the broader care continuum
- improving quality of care
- addressing concerns with performance, oversight and accountability
- developing new physical infrastructure
The government is investing $1.75 billion to create 30,000 modern long-term care spaces over ten years. Progress has already been made to update aging physical infrastructure by redesigning the funding model that supports the development of new spaces for residents. The modernized model provides tailored incentives to drive building in different markets and introduces an up-front development grant to address high cost barriers to construction. This will allow the government to create close to 11,000 safe, modern spaces over the next four years for residents to call home. New spaces will have better temperature control and will have no more than two residents per room, allowing for the phase out of rooms with three or four residents that have been so detrimental to fighting COVID-19 outbreaks.
To address another pillar of this aggressive modernization plan, the government has launched the Community Paramedicine for Long-Term Care Program as an innovative way to integrate long-term care services within the broader continuum of care. This program will provide enhanced at-home supports for Ontarians waiting to be placed in a long-term care home. It will help more seniors stay safe while living in the comfort of their own homes for a longer period of time.
Work is also underway to address the performance, oversight and accountability pillar through the development of a new quality framework. This framework will support quality assurance, continuous quality improvement and increased public transparency and it will contribute to an improved culture within long-term care.
With Ontario’s Long-Term Care Staffing Plan, the government is continuing the critical modernization work of ensuring residents receive the highest quality of care. This plan sets out actions and interventions to improve quality of care and quality of life for long-term care residents, while also making the sector a more desirable career destination.
A better place to live, a better place to work: Ontario’s long-term care staffing plan
The vision of this long-term care staffing plan is to support a qualified and engaged long-term care workforce with effective and accountable leadership to provide residents with a safe and supportive living environment. At the centre of this plan is the government’s commitment to increase the hours of direct care for residents to an average of four hours per day over four years. This will require the education and training of new professionals to fill more than 27,000 full-time equivalent jobs which will be needed to reach this standard.
Over the next four years, this government will increase investments in long-term care staffing annually, spending up to $1.9 billion in 2024–2025 to support increased staffing levels. Additional investments will be required to educate additional qualified individuals to fill these new positions.
The staffing plan focuses on six areas of action:
- increasing the hours of direct hands-on care provided by nurses and personal support workers, to an average of four hours per day per resident—including a significant increase in nursing care to reflect the acuity of long-term care residents; and expanding resident access to allied health staff like physiotherapists, occupational therapists and social workers
- accelerating and expanding educational pathways to help recruit the tens of thousands of new staff that will be needed
- supporting continued development and professional growth for long-term care staff, which will also improve retention
- improving working conditions for staff
- building effective and accountable leadership in homes across the province to improve oversight within homes, guidance and medical outcomes in long-term care homes
- measuring progress against key performance indicators
By addressing these staffing challenges, the government will improve resident quality of care, increase the ability of homes to recruit and retain high caliber staff, eliminate shortages and provide an enhanced workplace experience.
However, the government cannot do it alone. The province recognizes many long-term care homes are already leading through innovation and best practices and calls on sector partners to work together to make the critical changes that can only happen on the ground. The efforts of all partners–long-term care homes, professional associations, labour, regulatory bodies, education and training partners—will be needed to leverage the investments and initiatives in the staffing plan. Working together, the vision for a modern and safe long-term care sector can become a reality.
1. Increasing staffing levels
Addressing resident needs requires additional staff in homes to provide increased hands-on care. Through the 2020 Budget, Ontario’s Action Plan; Protect, Support and Recover, the government has committed to increasing direct care to an average of four hours per resident per day—making Ontario a leader in Canada by committing to this level of care. This is an increase of more than 45% from the most recent estimate of hours worked per day—an average of two hours and 45 minutes by personal support workers, registered nurses and registered practical nurses.
This commitment to a daily average of four hours of care per resident will include substantially increasing the amount of time that registered nurses, registered practical nurses and personal support workers have available for resident care. In particular, increasing nursing hours is needed due to the rising acuity of residents and will help to limit unnecessary, and potentially harmful, hospital transfers.
The government also plans to increase the hours of care provided by a broader range of staff who play a key role in supporting residents to achieve a higher quality of life and promoting good mental health. This includes supports provided by physiotherapists, occupational therapists, recreation therapists, social workers and others who can address physical, emotional, social and spiritual needs of residents.
To achieve this level of care, tens of thousands of new staff will need to be educated, trained and hired.
As promised, the government has set clear targets in this staffing plan. Progress will be measured against these targets and other factors listed below, to achieve this outcome by 2024–2025.
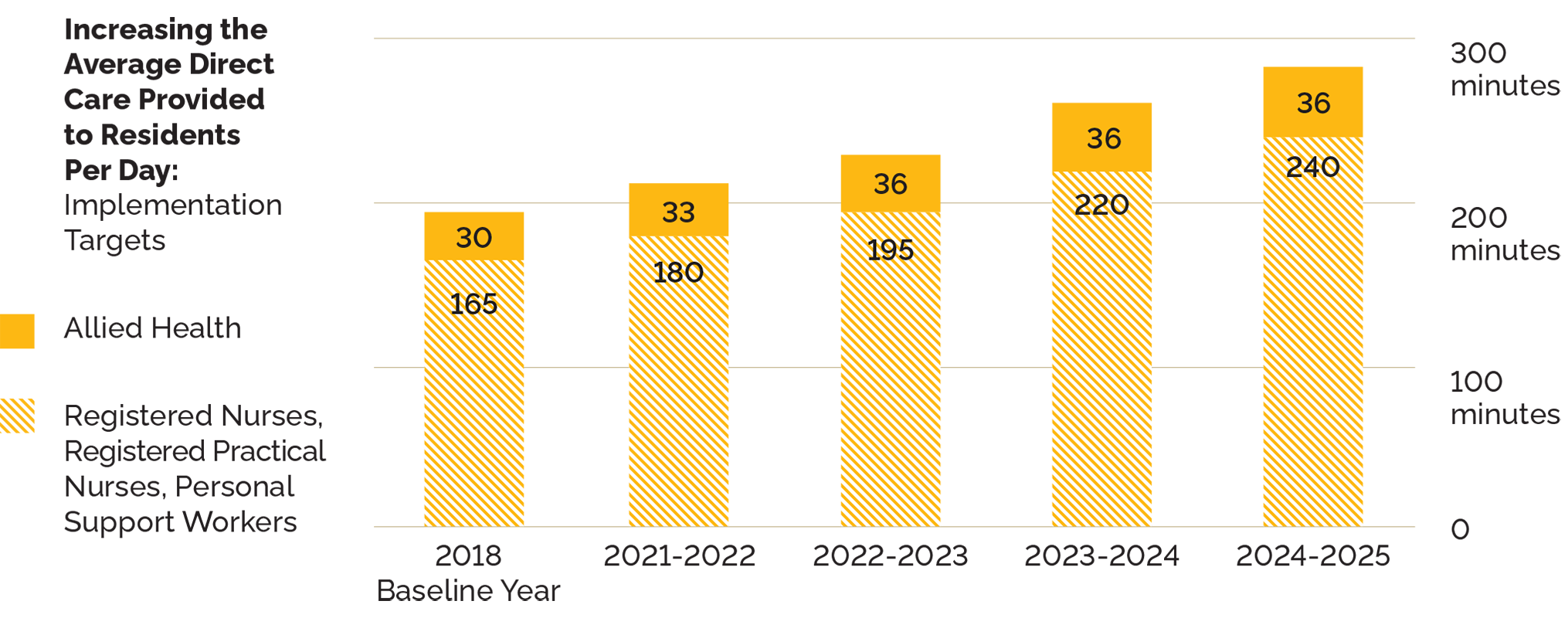
| Year | Registered nurses, registered practical nurses, personal support workers | Allied health |
|---|---|---|
| 2018 baseline year | 165 | 30 |
| 2021–2022 | 180 | 33 |
| 2022–2023 | 195 | 36 |
| 2023–2024 | 220 | 36 |
| 2024–2025 | 240 | 36 |
Increasing the hours of direct care provided to residents will improve health outcomes and working conditions, both of which will reduce stress and anxiety for staff and families. In addition, increasing broader supports will contribute to improved mental health and a higher quality of life for residents.
Initiatives
Immediate action: Enabling an average of four hours of direct care in four years
Staffing study recommendation
Investments into nursing and personal support to enable an increase of combined direct care hours provided by registered nurses, registered practical nurses and personal support workers from a daily average of two hours and 45 minutes worked per resident (2018) to a daily average of four hours. This will require hiring more than 27,000 registered nurses, registered practical nurses and personal support workers.
This investment will enable homes to increase their direct care hours, as well as increase their proportion of nursing professionals to reflect the rising acuity of residents.
Implementation targets for direct care hours:
- By the end of year 1: 3 hours
- By the end of year 2: 3 hours 15 minutes
- By the end of year 3: 3 hours 42 minutes
- By the end of year 4: 4 hours
Immediate action: Increasing therapy, social care and other supports for residents
Staffing study recommendation
Investment into allied health care workers such as physiotherapists and social workers to increase the average worked hours by 20% This will increase the homes’ capacity to tailor care plans to individual resident needs and support a more mobile and fulfilled resident population. This additional care time is the equivalent to 2000 new full-time positions, which will be carried out by a variety of workers across province.
Further action: Guidance to long-term care homes on staffing models
Gillese inquiry and staffing study recommendation
Each home needs some flexibility to recruit staff that meet each resident’s specific needs, which are diverse and unique.
Guidance may include:
- staff-to-resident ratios
- linking the requirement for 24/7 oversight by a registered nurse to the size of the home
2. Disrupting, accelerating and increasing education and training pathways
Planned government investments to increase staffing levels will create demand for tens of thousands of new jobs. The government knows some long-term care homes currently struggle to fill all their vacant nursing and personal support worker positions. While improvements to working conditions will help improve retention, traditional educational pathways at current enrolment levels will not be sufficient to create the supply of qualified health care professionals needed in long-term care.
That’s why the government will be working with partners to significantly scale up traditional pathways while also implementing new and innovative approaches, such as on-the-job training models, to develop the qualified personnel needed.
The initiatives below build on current programs aimed at filling immediate needs for frontline staff and are aligned with and supported by the broader Health Human Resources Strategy. Each initiative will help meet the significant additional demand created by the government’s commitment to increase care hours.
The government will work with partners in early 2021 to plan the education and training approaches needed for implementation, beginning in the 2021–2022 fiscal year.
Initiatives
Action taken: Stabilizing long-term care homes
To urgently address the need for more staff, the following programs have been developed and/or implemented to immediately educate, recruit and retain frontline staff in long-term care homes:
- Investment of $52.5 million to recruit, retain and support an additional 3,700 frontline health care workers, including in long-term care, to meet surging demand. This includes the following initiatives:
- Personal Support Worker Return of Service Program to attract trained personal support workers into long-term care
- Supportive Care Worker Program, which trains workers to provide basic home support services
- Personal Support Worker Fast Track, which will quickly train students with prior health care experience in a condensed personal support worker program
- Nursing Graduate Guarantee, which provides full-time salaries and benefits, with a focus on recruiting in areas of need, such as long-term care homes
- Ontario Matching Portal, launched in April 2020, has helped make over 660 staffing matches for long-term care to-date
- Recently announced Ontario Workforce Reserve for Seniors Program will help recruit, train and deploy individuals seeking new opportunities into long-term care homes as resident support aides during the pandemic. These aides will assist residents with various activities, such as support with technology and recreation.
- Investment of $20 million for additional infection prevention and control personnel.
- Additional
scale up
initiatives are planned and being developed for implementation. Together, these initiatives are intended to bring thousands of health care workers into the long-term care sector over the next few months.
Immediate action: Accelerating and disrupting education and training pathways
Staffing study recommendation
Building on current stabilization actions and other on-the-ground innovations, immediately create new, accelerated pathways to education. The ministry will bring together government and education, training and long-term care partners to drive change, including:
- internationally trained professionals: creating innovative pathways and removing existing barriers to enable more placements for internationally educated health care workers and students
- an
Earn-as you-Learn
personal support worker pathway: including on-the-job education, onsite training and micro-credentialing, with an opportunity to include retirement homes - registered practical nurse to registered nurse bridging: accelerating supply of registered nurses by supporting registered practical nurses who wish to transition into the registered nurse role
Immediate action: Scale up traditional education pathways
Staffing study recommendation
In addition to innovative and accelerated pathways, significant investments in traditional education and training streams will be needed in consultation with educational institutions to maximize potential supply for long-term care (for example, sizeable scale up in the number of education seats at colleges and universities). This will also help mitigate impact on other sectors that continue to have a strong demand for the same qualified personnel.
Further action: Awareness campaign
Staffing study recommendation
As new pathways and educational opportunities are created and working conditions in long-term care improve targeted awareness and recruitment campaigns will be developed and aimed at high school, college and university students, employment centers, newcomers and second career seekers.
3. Supporting ongoing staff development
The government is committed to supporting ongoing staff development and professional growth to help current long-term care workers acquire new skills and expertise over their career. This initiative will help improve the desirability of careers in long-term care and contribute to increased staff retention. The government recently provided $10 million for infection and prevention control training for staff and has established a training fund to start in 2021–22, to help homes back-fill staff while they attend professional training. Addressing staff preparedness and growth will contribute to improved retention by highlighting long-term care as a career destination—not a point-in-time job.
The government recently provided $10 million for infection and prevention control training for staff and has established a training fund to start in 2021–2022, to help homes back-fill staff while they attend professional training. Addressing staff preparedness and growth will contribute to improved retention by highlighting long-term care as a career destination—not a point-in-time job.
Initiatives
Action taken: Providing IPAC education and training
Staffing study recommendation
The government has invested $10 million to implement Infection Prevention and Control (IPAC) training for all new and current staff.
Immediate action: Supporting staff education and training
Gillese inquiry recommendation
Beginning in 2021–2022, the government will make a $10 million training fund available to support long-term care homes in back-filling positions for staff that attend in-person training sessions.
Further action
Working with sector leaders to build on existing innovations, the government will develop and implement initiatives that help new workers successfully transition into employment and help continuing employees experience career growth and satisfaction. This could include mentorships, preceptorships and communities of practice.
4. Improving working conditions
Improving working conditions is integral to addressing issues of staff retention and improving the conditions of care for residents.
The government’s commitment to significantly increase the level of direct care provided to residents through increased staffing will help address workload and burn-out issues for long-term care staff. Homes will be better resourced with more staff to share and complete tasks, leading to more timely, less rushed care.
As the government makes significant investments to increase staffing levels, sector partners need to help lead change in critical areas. While the province recognizes the scheduling challenges of a 24/7 environment, this change must include exploring and sharing best practices to increase full-time positions and employee retention.
Initiatives
Immediate action: Sector-led improvements
Staffing study recommendation
As an initial focus, the Ontario Long-Term Care Association and AdvantAge Ontario will lead a working group to identify opportunities, best practices and potential barriers to enhance scheduling methods and increase full-time positions.
The government will also work with our sector partners, including employers, associations and unions, to further address working condition issues.
Immediate action: Reducing administrative burden
Staffing study recommendation
The government will launch a technical working group with sector partners to review components of the long-term care funding model, focusing on two aspects of the funding formula:
- Case Management Index (CMI)
- High Intensity Needs Fund (HINF)
This funding model review would include understanding the impact of the funding formula, and resulting documentation requirements, on staff at a day-to-day level with the aim to return as much time as possible to direct care.
The short-term goal will be to identify concrete improvements that modernize the long-term care funding formula and reduce administrative burden, without reducing record keeping necessary for appropriate resident care. The review will also identify alternative approaches and longer-term strategies that may be appropriate from a clinical, funding and performance measurement perspective, as well as cost implications for the province.
Results of this review are expected to be available by the end of August 2021.
Further action: Working smart
Staffing study recommendation
The Ministry of Long-Term Care will work with the sector to better enable staff to spend more time on direct resident care, including through digital health tools and further opportunities to modernize the workplace.
Sector perspective
The backbone of our long-term care system is the thousands of dedicated staff who devote themselves to caring for residents who call it home. We can—and must—give them the support and time for more personalized care and meaningful engagement with residents. Enormous workloads and increasingly complex care needs place a huge mental, emotional and physical strain on front-line workers and make it very hard to attract and retain the right mix of qualified people. This commitment to achieve an average of four hours of care will mean more staff delivering more care, and that is what truly matters.
Jane Sinclair, General Manager, Health and Emergency Services, County of Simcoe
5. Providing effective and accountable leadership
Local leaders—such as administrators, medical directors and directors of care—play a crucial role in shaping workplace culture and fostering a collaborative, team-based environment built on a coherent philosophy of care. Many homes are part of a larger organization that owns multiple homes and sometimes other related services, such as a broader campus of care. In these cases, there are additional leaders—such as boards of governors, corporate or head office leaders—who also have an important impact at the local level. Effective and accountable leadership across long-term care is critical to supporting the staffing plan initiatives, achieving necessary culture change and ensuring residents receive a higher quality of care and life.
Initiatives
Action taken: Increasing nurse practitioners
Staffing study recommendation
The government is implementing the third phase of the Attending Nurse Practitioner in Long-Term Care Homes program, which provides annualized funding for up to 15 additional nurse practitioners to the sector.
Action taken: Supporting medical directors
The Ministry has worked with stakeholders to develop a guidance document to provide clarity on the role and responsibilities of existing medical directors and support them in preparing and responding to future waves of COVID-19.
Further action: Clarifying the role of Medical Director and assessing need for nurse practitioners
Staffing study recommendation
The Ministry will work with sector partners to clarify the role of key leadership positions, including administrators and medical directors, and to consider the further need for nurse practitioners.
Further action: Leadership onboarding, training and ongoing support
The government will work with sector partners to improve the training and onboarding that long-term care leaders (medical and otherwise) are required to complete. Topics could include infection prevention and control, emergency planning, philosophy of care, geriatric principles and human resources.
Sector perspective
With more than 20 years of experience in delivering training for new and aspiring long-term care leaders through our Administrator Leadership Program, we know that effective administrative and clinical leadership is integral to making long-term care a better place to live and work. Well prepared leaders can harness opportunities to tackle the challenges of today, while inspiring their teams to envision and embrace the future of seniors’ care.
Lisa Levin, CEO, AdvantAge Ontario
6. Measuring success
Successful implementation of this staffing plan will require an ongoing, concerted effort, as well as an ability to adjust course as needed. To ensure that the province achieves its targets, regular measurements will be required to track progress across the sector. As needed, the government will develop new tactics and course correct
along the way.
Initiatives
Immediate action: Enhanced data collection
The ministry will review and enhance the current staffing survey of long-term care homes and encourage stronger participation. Currently, an annual staffing report is a requirement in the service agreement between long-term care homes and the Local Health Integration Networks and Ontario Health.
Immediate action: Measure plan outcomes
The ministry will work with the sector to finalize outcomes and indicators to measure the success of the plan. This could include the amount of direct care provided by profession and resident/family and staff satisfaction.
Further action: Evaluate the plan’s success and report publicly
The ministry will report publicly against targets and outcomes annually, and formally evaluate progress in later years of the plan.
Working together to achieve meaningful change
To achieve the government’s vision, it is important to know what success looks like. Success is a 21st century long-term care sector that is resident-centered and provides access to the highest quality of care for our most vulnerable, when and where they need it.
The Long-Term Care Staffing Plan, with its interrelated initiatives, will lead to historic improvements in quality of life and care for residents, greater staff recruitment and retention in long-term care, and increased public confidence that long-term care homes are helping residents live safely and comfortably.
Overcoming the current, long-standing challenges in long-term care will require a sustained effort over the years ahead and close collaboration of all partners. The province calls on these partners to work together and make the critical changes that can only happen on the ground. The government knows these issues existed and started to address them before the COVID-19 pandemic, however, resolving them will take a sustained, collective effort over time.
The ambitious plan that the government has put forward targets deep-rooted and systemic issues. By addressing these staffing challenges, the province will improve resident quality of care, increase the ability of homes to recruit and retain high caliber candidates and eliminate shortages and provide an enhanced workplace experience for staff.
Working together with all partners, this vision for long-term care residents can be a reality, ensuring that long-term care homes are a better place to live, and a better place to work.
Sector perspective
The staffing crisis is a multi-faceted, cross-sectoral challenge that will take all of us—long-term care and government, as well as health system, labour and higher education partners—working together to ensure we can meet the needs of Ontario’s long-term care residents today and in the future
Donna Duncan, CEO, Ontario Long Term Care Association
Appendix: Prior accomplishments
Ontario is the only province in Canada that has a dedicated Ministry of Long-Term Care, established in 2019 to address long-standing and systemic issues that have existed for decades.
The government is taking action to create a 21st century long-term care sector that includes investing $1.75 billion to create 30,000 modern long-term care spaces over ten years, providing residents with a country-leading average of four hours of daily direct care, and ensuring that long-term care homes provide our most vulnerable with a comfortable and safe environment to call home.
COVID-19 has created unprecedented challenges across long-term care and other health sectors. It has disproportionately affected residents and staff at long-term care homes. The government’s top priority from the beginning of this pandemic was, and remains, to protect the health, safety and well-being of our most vulnerable residents and the heroic staff who care for them.
Ontario declared the province in a state of emergency on March 17, 2020. The government has acted swiftly and urgently address outbreaks and to support all long-term care homes, residents and staff—issuing several emergency orders, guidance documents and provincial directives, which have played a vital role in responding to this rapidly changing situation.
Specific actions include:
- Issued the first guidance to the long-term care sector on January 31, 2020, and it has been continuously updated since.
- Enhanced measures to enforce physical distancing and implemented a temporary order that gives homes the flexibility they need to deploy staff when and where they are most needed.
- Introduced directives that focused on keeping residents safe, which meant quickly and decisively limiting the flow of people in and out of homes.
- Enabled hospitals, public health units and the home care sector to deploy health professionals to homes experiencing critical staffing shortages.
- February 3, 2020—the Ministry of Health released guidance on COVID-19 prevention and screening in long-term care.
- March 9, 2020—the Ministry of Long-Term care issued guidance to all long-term care operators to actively screen all visitors, residents, re-admissions and returning residents to long-term care homes.
- March 16, 2020—The Chief Medical Officer of Health issued guidance to all Ontario long-term care homes to allow only essential visitors until further notice. Essential visitors are people visiting residents who are very ill or require end-of-life care.
- March 20, 2020—The Ministry of Long-Term Care amended regulations to allow for increased flexibility in staffing, making it easier for qualified staff to be hired and for homes to prioritize skills where they are needed most. These measures allowed for homes to quickly bring in more and new staff, to prevent potential staffing shortages and to allow staff to spend more time on direct care to residents.
- March 22, 2020—The Chief Medical Officer of Health issued a directive to long-term care homes to immediately implement precautions and procedures for short stay absences to visit family and friends. Under this directive, to minimize the risk of exposure to COVID-19, residents are not permitted to go outside of the home (except on the property of the home), and wherever possible, measures are put in place for staff to limit their number of different work locations.
- March 23, 2020—The Ministry of Long-Term Care issued a temporary order for long-term care homes to support increased staffing flexibility, enabling homes to be able to respond to, prevent and alleviate an outbreak of COVID-19
- March 30, 2020—The Chief Medical Officer of Health issued a directive for long-term care homes to immediately begin more aggressive screening—upgraded to twice daily—of staff, essential visitors and residents. The directive includes rigorous direction for staff and resident co-horting, the limitation of staff workplaces, COVID-19 testing and the latest protocol for outbreak management, among other critical guidance.
- April 15th, the Ministry of Long-Term Care issued a third emergency order that ensures that long-term care home employees only work in one health care setting, whether that is a long-term care home, retirement home, or other health care setting to help limit the spread of COVID-19. Additional resources and timeline.
- Invested $243 million in emergency funding, in the March spring economic statement, to cover the costs associated with screening, more staffing to support infection control, emergency capacity and supplies and equipment to help the sector tackle COVID-19 and protect our most vulnerable.
- The COVID-19 action plan for long-term care homes was implemented to create a roadmap and ramp up the protection of long-term care residents and staff. The Action Plan included aggressive measures for more extensive testing, screening and surveillance—leading to virtually all residents and staff in long-term care homes being tested for COVID-19.
- Called on the Canadian Armed Forces to provide temporary support at seven long-term care homes to ensure the ongoing safety of residents and maintain effective staffing levels.
- Introduced temporary pandemic pay on April 25, 2020 to help frontline staff who experienced severe challenges in the workplace and were at heightened risk during the COVID-19 outbreak. Eligible workers in long-term care received additional payments of $4 an hour on top of their regular wages. In addition, eligible workers that worked 100 or more hours in designated four-week periods received $250 per four-week period, up to $1000. This benefited approximately 100,000 full-time, part-time, casual, clinical and support staff and was effective for 16 weeks, from April 24, 2020 until August 13, 2020.
- In May, implemented alternative management support from local hospitals at 20 long-term care homes to help them respond to and manage COVID-19 outbreaks. Homes are also partnered with local hospitals so that in the event of an outbreak, there is additional support to help them contain the spread of COVID-19 and return them to normal operations.
- Carried out sector preparedness assessments to help long-term care homes with emergency and outbreak prevention and management planning in anticipation of future COVID-19 waves. Long-term care homes were encouraged to work with their partners (for example, hospitals, public health units) and Ontario Health regions to conduct preparedness assessment exercises to help identify any gaps in preparedness planning.
- Invested over half a billion dollars in additional funding to protect our most vulnerable seniors and those who care for them during the second wave of COVID-19. This was part of the provincial COVID-19 fall preparedness plan—Keeping Ontarians safe: preparing for future waves of COVID-19—and informed by key themes that emerged from the sector preparedness assessments—such as staffing challenges, the importance of infection prevention and control and strengthened partnerships.
- Established an independent commission to investigate how COVID-19 spread within long-term care homes, how residents, staff and families were impacted, and the measures taken by the province and other parties to prevent, isolate and contain the spread. The commission will offer guidance on how to better protect long-term care home residents and staff from any future outbreaks.
- Introduced a temporary wage increase of $3 per hour for approximately 50,000 eligible workers who deliver publicly funded personal support services in long-term care, effective October 1, 2020.
Appendix: Direct hours of care results and progress plan
September 27, 2024
Leading Canada in long-term care
Ontario is a national leader in long-term care. Ontario has made unprecedented investments to fix the long-term care system — from building modern, safe, and comfortable homes, to connecting seniors with faster and more convenient access to the services they need.
Since becoming its own ministry in 2019, the Ministry of Long-Term Care has achieved significant progress. In 2020, as part of its commitment to improve long-term care services, the government released the Long-Term Care Staffing Plan, which included public commitments to improve Ontario’s Long-Term Care system and set the framework for legislated direct care targets.
The Fixing Long-Term Care Act, 2021 came into force on April 11, 2022. The legislation contains several measures to improve staffing and care, including two sets of legislated, provincewide, system-level targets.
The legislation set a historic goal to provide an average of four hours of direct care per resident, per day by nurses and personal support workers — enshrined in legislation. The government backed this goal with record investments in:
- training
- education
- recruitment
- recruitment and retention incentives
Today, the province has met 93% of its goal, and continues in its unwavering commitment to providing safe, high-quality direct care for its most vulnerable residents.
Growing the direct hours of care
Since 2020, the Ontario government has been driving increased hours of direct care through direct investments like training and education programs, promotions and incentives designed to bring thousands of new workers into the long-term care sector.
Investments
Since 2020–2021, the province has allocated more than $4.9 billion in dedicated funding to achieve its care goals, including a historic investment of $1.82 billion in 2024–2025.
Among the early investments was a wage increase for personal support workers (PSWs). In 2020, the government implemented a temporary wage increase of $3 per hour for publicly funded PSWs — and made the increase permanent in 2022. Today, approximately 53,000 eligible long-term care PSWs are benefiting from the increase.
Training and education
Robust training and education programs are vital for building a skilled, professional workforce.
Ontario’s broad range of training options ensure that people have multiple pathways into long-term care — and offerings beyond the entry level demonstrate that they can have fulfilling careers in the sector, with opportunities for personal and professional advancement.
Between 2020 and 2024, approximately 24,000 more PSWs and 3,000 more nurses graduated through targeted investments in collaboration with educational institutions.
Alongside these academic education programs, Ontario invests in other training supports, including:
- the Living Classroom program in which students train to become PSWs on-site in local long-term care homes across Ontario
- the Preceptor Resource and Education Program for Long-Term Care (PREP LTC) — which supports successful clinical placements, has helped more than 500 long-term care homes provide clinical placements for more than 19,000 PSW and nursing students since 2022
- bridging programs, in English and French, that help employees upskill -
- from general employees to become PSWs
- from PSWs to registered practical nurses
- from registered practical nurses to registered nurses
- the Supporting Professional Growth Fund, launched in 2021, which supports ongoing education and training for more than 45,000 eligible staff in long-term care homes
Recruitment and retention
In November 2023, the government introduced incentives of up to $25,400 for PSW students and recent graduates:
- student fees waived for PSW students learning through district school boards
- up to $5,400 for students as they complete their clinical placements
- $10,000 to recent graduates who commit to working in a long-term care home for 12 months, and a further $10,000 if the home or provider is in a rural, remote or northern location
Other measures have also helped grow the staffing pool. For example:
- 1,000 internationally educated nurses have become qualified registered nurses in Ontario with the support of the Supervised Practice Experience Partnership Program in Long-Term Care.
- Since 2022, almost 137 additional nurse practitioners full-time equivalent positions have been added across 139 long-term care homes under the Hiring More Nurse Practitioners for Long-Term Care initiative.
Milestone results
The Ontario government’s care commitment sets goals for 2 groups of care providers:
- nurses and PSWs — an average of 4 hours of direct care per resident per day
- allied health professionals (such as resident support personnel, social workers, physiotherapists and occupational therapists) — an average of 36 minutes of direct care per resident per day
The Fixing Long-Term Care Act, 2021 lays out annual milestones leading up to the 2024–2025 targets.
Targets for year 1 (2021–2022)
- Allied health professionals (AHPs): 33 minutes of direct care per resident, per day
- PSWs/Nurses: 3 hours of direct care per resident, per day
Targets for year 2 (2022–2023)
- AHPs: 36 minutes of direct care per resident, per day
- PSWs/Nurses: 3 hours, 15 minutes of direct care per resident, per day
Targets for year 3 (2023–2024)
- AHPs: 36 minutes of direct care per resident, per day
- PSWs/Nurses: 3 hours, 42 minutes of direct care per resident, per day
Targets for year 4 (2024–2025)
- AHPs: 36 minutes of direct care per resident, per day
- PSWs/Nurses: 4 hours of direct care of direct care per resident, per day
As of August 30, 2024, Ontario is 93% of the way to its goal for nurses and PSWs. It has exceeded its targets for allied health professionals every year. In total, the province has provided more than an hour of additional direct care to Ontario’s long-term care residents through this government’s unprecedented investments. This is a 33% increase in direct care since 2021.
In the first quarter of Year 4 Ontario exceeded its Year 3 direct hours of care target.
Charting the course to the finish line
Ontario has exceeded the target for care provided by allied health professionals every year since 2021–2022. The focus is on sustaining progress on the allied health professionals target and bringing the average direct hours of care provided by nurses and PSWs to the four-hour mark.
Challenges that must be addressed include:
- lingering impacts of the COVID-19 pandemic
- global health human resource shortages and inflationary pressures
- the growing aging population, many with increasingly complex needs
The Ontario government’s plans to overcome these challenges include:
- boosting investments still higher — in the 2024 Budget, the government announced a 6.6% increase ($352.9 million) in level-of-care base funding, on top of the $571 million of funding already earmarked for the sector in 2024–2025 to help achieve the Year 4 targets
- further expanding training and education programs that are supporting upskilling and clinical placements
- enhancing outreach — raising awareness of opportunities and attracting more people to working in long-term care
Conclusion
The Ontario government launched the historic four-hour average daily direct care goal as part of its broader plan to fix long-term care. Today, we are 93% of the way there, and driving forward to deliver on our commitment.
At the same time, we continue to engage stakeholders, partners, health service providers and, most importantly, long-term care residents and families, to transform the long-term care sector for the better.
Ontario is working to ensure residents get the care they need and deserve, now and in the future. Our priority remains ensuring the health, safety, and well-being of all residents in our long-term care homes.
Year 4: Direct hours of care results and progress plan
August 1, 2025
Ontario's commitment to care
Ontario continues to be a national leader in long-term care. It is the only province in Canada to set direct hours of care (DHOC) targets in legislation and publicly share information on results, underscoring Ontario’s leadership and commitment to improving resident-centred care.
The government’s four-year staffing plan, A Better Place to Live, a Better Place to Work, concluded on March 31, 2025. The plan was established to increase staffing levels, improve working conditions and strengthen education and training pathways in Ontario’s long-term care sector.
At the heart of this plan is a commitment to establish an average of 4 hours of care per resident, per day, delivered by nurses and personal support workers (PSWs), along with an additional 36 minutes by allied health care professionals (AHPs), as outlined in the Fixing Long-Term Care Act, 2021.
Target dates were set to improve daily direct care time for long-term care residents:
- As of March 31, 2023, AHPs are expected to deliver at least 36 minutes of daily direct care per resident.
- By March 31, 2025, nurses and PSWs must provide 4 hours of direct care per resident each day.
The government backed this goal with record investments in:
- training and education
- recruitment and retention incentives.
As of March 2025, the province has met 95.5% of its goal, up 8% from last year and continues to provide safe, high-quality direct care for its residents.
Progress
Ontario continues to make significant progress toward improving daily care for long-term care residents:
- In Year 4 of the staffing plan (2024 to 2025), the province achieved 95.5% of its goal to provide an average of 4 hours of direct daily care by nurses and PSWs — an 8% increase over the previous year.
- From January to March 31, 2025, performance surged to 98% of the Year 4 target — meaning that long-term care residents are receiving more direct care since measurement began.
- For the fourth consecutive year, Ontario exceeded its target of 36 minutes of daily direct care from AHPs.
- Since 2021, long-term care residents have received, on average, more than an hour of additional daily direct care — a 36% increase which is equivalent to 15 days of additional care per resident.
Investments in the workforce
Since 2020, Ontario has made historic investments to grow and retain the workforce in long-term care homes. The government has allocated $4.9 billion over 4 years to:
- increase staffing numbers
- enhance care
- ensure residents receive the support they need
Training and education
As part of its efforts to build a skilled workforce, Ontario continues to invest in training and education programs that make long-term care a viable and rewarding career path. As a result:
- More than 24,000 PSWs and 3,000 nurses were trained through targeted investments between 2021 and 2024.
- Over 35,500 student placements were supported through the Preceptor Resource and Education Program in Long-Term Care (PREP LTC).
- More than 1,100 PSW students across the province enrolled in 49 Living Classrooms during the first 2 years of the program.
- More than 600 long-term care staff upskilled into PSW roles with support from the Learn and Earn initiative.
- 236 PSWs and 545 nurses have enrolled through partnerships with Indigenous Institutes since 2021.
- The BEGIN (Bridging Education Grant in Nursing) Program has funded over 1,300 students in registered practical nurse (RPN) and registered nurse (RN) programs who have pledged to working in long-term care following graduation. More than 580 have started working in the long-term care sector.
Recruitment and retention
Ontario has implemented targeted strategies to recruit and retain staff.
- Nearly 1,500 PSWs have been hired in long-term care through the PSW incentives program. Eligible PSWs can receive up to $30,000 for committing to work in long-term care or home and community care.
- Over 190 nurse practitioner (NP) full-time equivalents were supported by the Hiring More Nurse Practitioners for LTC Program as of July 2025.
- Long-term care homes trained more than 45,000 existing staff through the ministry’s Supporting Professional Growth Fund between 2022 and 2024.
- The ministry permanently increased the wages of publicly funded PSWs by $3 per hour in 2022. Currently, approximately 58,000 PSWs in long-term care continue to benefit from this increase.
Next steps
Ontario continues progressing towards the legislated targets. This includes addressing the challenges that affect the government’s ability to recruit and retain qualified care staff at a pace that keeps up with the need of the province’s aging population. These challenges are further compounded by the construction of a record number of new and upgraded long-term care beds, an important government priority that will require even more staff to meet demand.
To build on the gains achieved to date, Ontario must address several persistent, sector-wide challenges, including:
- ongoing global health human resource shortages and inflationary pressures
- competition for existing and new staff from primary care, home care and hospitals
- ongoing difficulties recruiting and retaining staff in some rural and remote communities
Addressing challenges and advancing progress
The government will continue to address these challenges by focusing on the investments and actions that have driven our successes to date, such as:
- expanding recruitment, education pathways and partnerships to help more people find careers in long-term care, and increase our sector’s health human resources
- supporting system-wide sustainability by collaborating with other sectors to develop and implement strategies aimed at increasing health human resources
- improving retention through initiatives including incentives, mentorship programs and modernized working conditions that make the sector a more attractive and supportive place to work.
Conclusion
Ontario’s four-year staffing plan has driven significant progress, positioning the sector just shy of the legislated direct hours of care targets. Between January and March 31, 2025, the province achieved 98% of the four-hour target for nurses and PSWs and exceeded the allied health professionals’ targets for the fourth consecutive year.
The government will continue to build on this momentum with new investments, expanded programming, and by strengthening both new and existing partnerships. We are also leading by example as the only province with legislated DHOC targets. With this progress, we will continue to support homes, monitor progress and improve staffing outcomes.
This work to improve long-term care is part of the government’s plan to protect Ontario by ensuring the province’s most vulnerable get the quality of care and quality of life they need and deserve.