Ontario Take-Home Naloxone Programs
Learn how your organization or pharmacy can apply to distribute take-home naloxone and what additional resources are available.
This information is intended for those who work for or with the Ontario Naloxone Program (ONP) and the Ontario Naloxone Program for Pharmacies (ONPP).
Overview
Naloxone is a drug that can temporarily reverse an opioid overdose.
The Ontario Naloxone Program distributes injectable and nasal spray naloxone kits through participating community-based organizations to:
- individuals at risk of opioid overdose
- the individual’s friends and family
Through participating pharmacies, the Ontario Naloxone Program for Pharmacies distributes injectable and nasal spray naloxone kits to:
- individuals at risk of opioid overdose
- the individual’s friends, family, or other individuals in a position to assist the individual at-risk
Program eligibility
The following organizations, centres and programs are eligible to participate in the Ontario Naloxone Program:
- needle syringe programs
- hepatitis C programs
- public health units
- Aboriginal Health Access Centres
- AIDS service organizations
- Community Health Centres
- outreach programs
- withdrawal management programs
- shelters
- hospital emergency departments, urgent care centres and inpatient units
- police, fire services and St. John Ambulance branches are eligible to receive naloxone for use when responding to opioid overdoses
To participate in the Ontario Naloxone Program, your organization, centre or program must:
- be formally incorporated as an organization
- reach individuals at risk of opioid overdose, and their friends and family
- have demonstrated staffing capacity to manage distribution and training with clients, inventory and reporting requirements
Community pharmacies interested in distributing naloxone kits in the pharmacy may be eligible to participate in the Ontario Naloxone Program for Pharmacies.
Ineligible organizations: Businesses
Businesses are not eligible to receive publicly- funded naloxone through the Ontario Naloxone Program or Ontario Naloxone Program for Pharmacies.
Instead, businesses can purchase naloxone kits directly from the manufacturers.
How to apply
Ontario Naloxone Program
To apply to the Ontario Naloxone Program, your organization, centre or program administrator should contact your local public health unit.
Ontario Naloxone Program for Pharmacies
To participate in the Ontario Naloxone Program for Pharmacies, pharmacies must review all Executive Officer (EO) Notifications and Q and A’s outlining all the necessary information to participate.
Disclaimer
If you require the EO Notices and Q and A’s in an alternative format, please contact publicdrugprgrms.moh@ontario.ca. We will:
- acknowledge your request within three business days
- provide you with the content within 15 business days
How to be added to the naloxone kit locator map
Pharmacies and community-based organizations, centres and programs are encouraged to review the current map locator tool regularly to check if they are listed. The tool is updated regularly.
Pharmacies
If you would like to be added or removed from the map locator tool, please email PublicDrugPrgrms.moh@ontario.ca.
Community-based organizations
If your organization would like to be added to or removed from the map locator tool, please email ONP@ontario.ca.
For either request, please provide:
- your name
- your pharmacy or organization name and full address, including contact information (for example, email, phone, fax)
Naloxone administration training
Ontario Naloxone Program
Your organization, centre or program staff is responsible for training eligible individuals how to recognize and respond to an opioid overdose and how to administer naloxone.
Public Health Units provide guidance on this training.
Training will include how to recognize an opioid overdose and 5 steps to respond to an opioid overdose.
If you are with someone who is having an opioid overdose
- Shout their name and shake their shoulders.
- Call 9-1-1 if they are unresponsive.
- Give naloxone
- if using an injectable kit — inject 1 vial or ampoule (a small glass container) (0.4 mg/1 mL ) of naloxone into their arm or leg
- if using a nasal spray kit — lay the person on their back, insert the tip of nozzle into one nostril and press the plunger firmly
- Perform rescue breathing and/or chest compressions.
- If there is no improvement after 2–3 minutes, repeat steps 3 and 4. Stay with them.
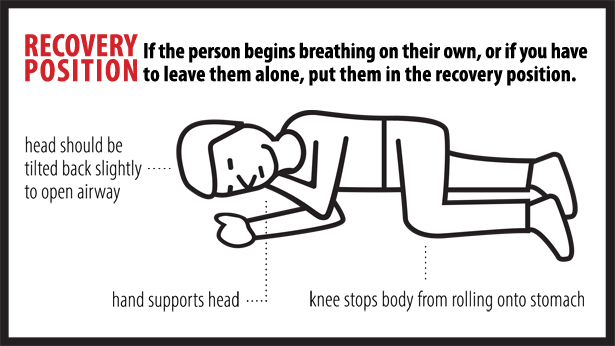
If the person begins breathing on their own, or if you have to leave them on their own, put them in the recovery position.
Stay until the ambulance arrives in case paramedics need help or information, or the overdose symptoms return. With more powerful opioids (fentanyl and carfentanil) there is a possibility that a person will overdose again even after they have been given naloxone and even if they don’t use more drugs.
Ontario Naloxone Program for Pharmacies
For those who receive a naloxone kit from a pharmacy, a pharmacist is expected to provide the necessary professional training to the eligible individual. Review all EO Communications and Q and A’s related to naloxone for details.
What’s in a naloxone kit
Each nasal spray naloxone kit includes:
- 1 hard case (for example, a zippered hard black case with red “naloxone” cross)
- 2 doses of naloxone hydrochloride intra-nasal spray (4 mg/0.1 mL))
- 1 rescue breathing barrier
- 1 pair of non-latex gloves
- 1 card that identifies the person trained to give the naloxone
- 1 insert with instructions (English and French)
Each injectable naloxone kit includes:
- 1 hard case (for example, a zippered hard black case with red “naloxone” cross)
- 2 (0.4 mg/1 mL) vials or ampoules (a small glass container) of naloxone
- 2 safety-engineered syringes with 25g, 1” needles attached
- 2 alcohol swabs
- 2 devices (known as “breakers,” “snappers,” or “openers” for opening ampoules safely)
- 1 rescue breathing barrier
- 1 pair of non-latex gloves
- 1 card that identifies the person who is trained to give the naloxone
- 1 insert with instructions (English and French)
Information for participating pharmacies
Through the Ontario Naloxone Program for Pharmacies (ONPP), participating pharmacies can distribute publicly-funded injectable naloxone kits or nasal spray naloxone kits for eligible individuals.
Pharmacies are to procure pre-made naloxone kits and/or the required supplies to assemble the naloxone kits through their usual suppliers. The naloxone kit shall be assembled by a pharmacist or a person under the supervision of a pharmacist.
The Ontario Pharmacists Association has developed resources relating to naloxone kits, including a listing of kit contents.
Number of naloxone kits that can be distributed through the ONPP at one time
Through the Ontario Naloxone Program for Pharmacies (ONPP), eligible individuals may receive up to two naloxone kits (total 4 doses) per day.
Requirement to show Ontario health card at a participating pharmacy to receive a naloxone kit
An Ontario health card is not required to receive free naloxone kits from a participating pharmacy.
While a health card is not required, pharmacists should make reasonable efforts to obtain an Ontario health card number when providing a naloxone kit.
Expired or unused naloxone kits
Naloxone kits that are expired or unused can be brought to any pharmacy for safe disposal in Ontario.
Individuals, including patients, are encouraged to talk to their pharmacist about disposal of unused or expired medications, that may include unused or expired naloxone kits. Most Ontario pharmacies are able to accept such medications, as well as sharps (for example, needles and syringes).
Naloxone kits for individuals using prescription opioids
It is important that you discuss overdose risks with your patients. If you have concerns about a particular patient who may be at risk of overdosing, consider discussing with the patient about getting a naloxone kit and the applicable training. If your pharmacy does not participate in the ONPP or is not able to provide a naloxone kit, you can direct the patient to the government’s naloxone programs web page to find the nearest naloxone kit distribution site.
Pharmacists are expected to use their professional judgement when distributing naloxone kits and providing training as appropriate.
Legal protections
Canada’s Good Samaritan Drug Overdose Act, provides some legal protection for people seeking emergency help during an overdose.
In addition, Ontario’s Good Samaritan Act, 2001 provides some legal protection to individuals from civil liability in certain cases, such as if a person administers naloxone to a person experiencing an overdose in certain situations.
Provincial regulations regarding the administration and/or distribution of naloxone in Ontario
Injectable naloxone (0.4 mg/1 mL) and nasal spray naloxone (4 mg/0.1 ml) are behind-the-counter products available without a prescription in Ontario, when indicated for emergency use for opioid overdose. The dispensing of naloxone in an Ontario pharmacy is subject to the Drug and Pharmacies Regulation Act and the policies of the Ontario College of Pharmacists.
Resources
Download a free poster informing your clients or patients about the nearest place to get a naloxone kit.
- Poster - "Naloxone kits available here. Ask for one."
- Poster - "Naloxone kits available here. Ask your pharmacist".
In-person substance use and alcohol support
ConnexOntario
Ontario funds a wide range of community-based mental health and addictions programs and services through the Ontario Health regions. You can find more information about services in communities across Ontario through ConnexOntario.
ConnexOntario provides free and confidential information those in need of mental health and/or addiction support.
You can contact ConnexOntario by either:
- live chat and directory of services
- phone:
1-866-531-2600 (toll-free) - email: www.connexontario.ca/en-ca/send-email
- text/SMS: CONNEX to 247247
ConnexGo app: available on Android (Google Play) or iOS (App Store).
Youth Wellness Hubs Ontario
Youthhubs.ca offers:
- easily, accessible services for youth aged 12– 25 and their families (designed with youth, for youth)
- convenient and faster access to Integrated Youth Services (IYS) including mental health services, support for substance use concerns, primary health care, social services, housing, employment and more with a network of 32 hubs across Ontario serving more than 30 communities
- services that are free and range from low to high intensity supports including rapid walk-in services, booked appointments and virtual services
RAAM clinics
Visit a Rapid Access Addiction Medicine (RAAM) clinic. RAAM clinics help people seeking treatment for substance use issues, including opioids, alcohol and other substances. You do not need a referral or appointment to visit a RAAM clinic.
Doctors and counsellors at RAAM clinics help stabilize clients before referring them to primary care and other longer-term community mental health and addictions services and supports.
RAAM clinics can provide:
- assessments and diagnoses for substance use disorders
- treatment options
- prescriptions for medications to help with cravings and withdrawal symptoms
- counselling
- overdose prevention education
All clinics are:
- accessible on a walk-in basis, with patients typically seen within a few days of contacting the clinic
- client-centered
- non-judgmental