Appendices
Appendix a: CPRI’s domains framework overview
CPRI developed a framework for organizing, interpreting and communicating the large quantities of data provided by the interRAI child/youth suite assessments into meaningful topic areas.
- Safety
- The Safety domain addresses the control of hazards and assesses a young person’s risk in key areas. By understanding any dangers present, safety planning can focus on creating safe and secure environments which are important to foster good mental health.
- Family Life & Social Integration
- The Family Life and Social Integration domain captures valuable information on household composition, strong and positive relationships, and social opportunities. When issues are identified in this area, support can be put in place to help achieve stability within the young person’s familial and social interactions.
- Health Promotion
- The Health Promotion domain addresses any conditions that have an impact on a young person’s optimal level of health and wellbeing. By addressing these needs, we aim to invest in the young persons’ developmental potential by establishing lifelong health behaviours that promote competency and resilience.
- Functional Status
- The Functional Status domain highlights the young person’s ability to perform activities, manage routines, and participate in life situations. Addressing needs in this domain is important to help children and youth to reach their full potential in daily functioning.
- Services & Supports
- The Services and Supports domain identifies areas of need where additional services and supports can be beneficial. Addressing service and support needs early benefits the young person by providing tools for long-term success.
Appendix a: CPRI’s domains framework
interRAI ChYMH and ChYMH-DD components mapped to CPRI’s domains framework
ChYMH Assessment Sections:
| ChYMH-DD Assessment Sections:
|
ChYMH CAPs:
| ChYMH-DD CAPs:
|
ChYMH Scales:
| ChYMH-DD Scales:
|
ChYMH Assessment Sections:
| ChYMH-DD Assessment Sections:
|
ChYMH CAPs:
| ChYMH-DD CAPs:
|
ChYMH Scales:
| ChYMH-DD Scales:
|
*CPRI-designed enhancements to standard interRAI ChYMH or ChYMH-DD assessments
ChYMH Assessment Sections:
| ChYMH-DD Assessment Sections:
|
ChYMH CAPs:
| ChYMH-DD CAPs:
|
ChYMH Scales:
| ChYMH-DD Scales:
|
ChYMH Assessment Sections:
| ChYMH-DD Assessment Sections:
|
ChYMH CAPs:
| ChYMH-DD CAPs:
|
ChYMH Scales:
| ChYMH-DD Scales:
|
*CPRI-designed enhancements to the standard interRAI ChYMH or ChYMH-DD assessments
ChYMH Assessment Sections:
| ChYMH-DD Assessment Sections:
|
ChYMH CAPs:
| ChYMH-DD CAPs:
|
ChYMH Scales:
| ChYMH-DD Scales:
|
*CPRI-designed enhancements to the standard interRAI versions of ChYMH or ChYMH-DD assessments
Appendix b: getting started with selecting the right tools for your organization’s needs
Section 1.1: The interRAI ChYMH suite
gave an overview of key considerations when reviewing the assessments. Now that you have reviewed this section of the toolkit and looked at the ChYMH Suite tools on interRAI.org, it’s time to start thinking about your organization’s needs. Consider…
- What tool(s) might be the best fit for the entire organization?
- Are there particular considerations for your intake department?
- What about any program-specific needs?
“What Does the Research Show”
in the Overview and Background section summarizes some key points about implementation science. How will your organization incorporate this knowledge into your implementation planning? For example, how will you avoid taking an approach that focuses too heavily on setting guidelines and policies? How will you make sure your organization commits to a long-term plan?
Appendix c: guiding questions to support mapping
The following questions will guide your efforts to define your information needs and decisions about when and where to use the tools you have chosen. Engage program managers or direct care staff to determine processes that are realistic and likely to succeed. For each step, gather information, consider examples and other relevant factors and then make notes for your own plan.
| Step: | Ask: | Consider: | Plan: |
|---|---|---|---|
| 1 |
|
| |
| 2 |
|
| |
| 3 |
|
| |
| 4 |
|
| |
| 5 |
|
| |
| 6 |
|
| |
| 7 |
| Consider what can stay the same and what will need to change.
| |
| 8 |
|
|
Appendix d: is your leadership team ready to support staff through ChYMH suite implementation?
Use these prompts to think about your organization’s leadership team and whether it is ready to provide strong, consistent, and united support to staff through the ChYMH Suite implementation process. This is a crucial step – if the answer to any of these considerations is “no”, managers and supervisors will not have the knowledge, tools, skills, or motivation to aid in implementing the change. Using this tool can help you can identify any gaps and create a plan to bridge or eliminate them.
| Self-assessment reflection question | Response (Yes, No, Partially) | Plan to bridge or eliminate gaps |
|---|---|---|
| Do managers and supervisors understand what is required of them as the organization moves towards implementing the interRAI ChYMH Suite, including the specific actions and behaviours needed from them to support launching the tools (e.g., to introduce and follow through on new procedures)? | ||
| Have managers and supervisors been provided with the skills and tools to be successful at leading their staff though the implementation process (such as change management training)? | ||
| Is there a plan for managers and supervisors to monitor and support clinical staff in ongoing use of the tools (such as review of tool use added to supervision meetings)? If not, what could that look like in your organization? |
Appendix e: leadership activities planning
In this activity, key tasks for leaders identified through implementation science research have been applied to ChYMH Suite implementation. This list is not exhaustive nor required. Add or subtract from the list according to the unique circumstances of your organization.
| Task | Person(s) Responsible | Planned Timeline | Planned Approach |
|---|---|---|---|
| Form ChYMH Suite Implementation Team and ensure Terms of Reference includes communication protocols to provide feedback up to higher levels. |
| ||
| Develop/revise policies and procedures to support the changes being implemented. |
| ||
Speak about the importance of the initiative to:
|
| ||
Solicit and analyze feedback from:
|
| ||
| Use feedback and data to make adjustments and improvements to implementation efforts. |
| ||
| Reduce internal barriers such as duplication between ChYMH Suite assessments and internally developed information gathering tools, time constraints that impede learning, or issues with embedding ChYMH Suite assessment results into clinical decision-making. |
|
| Task | Person(s) Responsible | Planned Timeline | Planned Approach |
|---|---|---|---|
| Address system-level issues that affect work within the organization. |
| ||
| Engage with others outside of the organization (such as partner organizations, funders) to nurture champions and supporters. |
|
| Task | Person(s) Responsible | Planned Timeline | Planned Approach |
|---|---|---|---|
| Create data systems to support organizational decision-making (such as use of ChYMH Suite data to support administrative decision-making, use of metrics to evaluate implementation progress and success). |
| ||
| Create data systems to support clinical decision-making (such as ensuring that ChYMH Suite assessment results are used in treatment planning and evaluation). |
| ||
| Create data systems to support assessor competence and fidelity. |
| ||
| Create communication systems that ensure data is meaningfully and regularly shared with relevant audiences (such as staff, families, other stakeholders). |
|
Appendix f: risk management planning
This tool should be completed during the Planning phase to identify current risks and prepare for potential future risks. It is also useful to revisit this tool regularly throughout the implementation process to monitor the ongoing risks and provide an opportunity to flag new issues as they arise. We have pre-populated the first two rows with examples to show how this tool can be used. Add as many rows as needed for additional risks.
| Risk | Indicators | Potential Impact (High, Medium, Low) | Current Status (Green, Yellow, Red) | Owner | Mitigation Plan | Actions Needed |
|---|---|---|---|---|---|---|
| For example: Internet access not consistent for all staff | Staff unable to access online software | High |
| IT lead | Create “hoteling stations” for staff internet access or develop procedures for offline tool use | Complete assessments by hand or offline and use software at hoteling locations |
| For example: Not all staff available for scheduled training dates | Staff untrained by “Go Live!” date | Low |
| Training lead | Have staff trained as trainers | Train internally when staff are available |
Appendix g: communication plan template
This template follows CPRI’s 3-Step Process for Communication Planning, described in section 2. Use the prompts to prepare a targeted communication plan for each stakeholder and message. Add as many lines as needed. Communication Planning is not a one-time process, so be sure to review and add to this plan regularly.
| Identify your stakeholders | Consider their unique needs | Content | Lead | Plan for Two-Way Communication | Resources/ Costs Involved | Expected Outcome of the Message | Date/Timing | Monitoring/Evaluation |
|---|---|---|---|---|---|---|---|---|
| Consider direct and indirect stakeholders. | What is their current context /what do they already know? | What is the message? | Who will deliver the message? How? | How will we get feedback? | Do we need to involve other people/processes? | What is the purpose? | When will this be shared? | How will we know it was effective? |
Appendix h: training planning worksheet
Follow these steps to create a training plan that matches your organization’s needs and resources.
A. Determine volume of assessors to be trained
1. Think of the programs that are implementing the ChYMH Suite. How frequently are assessments expected to be completed on clients?
| Estimated monthly frequency | Notes | ||
|---|---|---|---|
| ChYMH-S: | |||
| ChYMH: | |||
| ChYMH-DD: |
2. Assessors should complete a minimum of 3 assessments per month to maintain skills.
Considering this and the projected volume of assessments above, how many assessors will you need, and who will the assessors be? Do you need to consider turnover for these roles?
| Estimated number of assessors | Notes | ||
|---|---|---|---|
| ChYMH-S: | |||
| ChYMH: | |||
| ChYMH-DD: |
3. Will any assessors use multiple tools?
- Yes
- No
- If yes, note predicted overlap:
B. Determine training delivery logistics
1. Determine training modality:
- In-person
- Web-based
2. Set standards:
(Refer to guidelines and recommendations in Section 2)
| Class size: | Minimum: _____ Maximum: _____ |
|---|---|
| Trainer Ratio: | (e.g., 2 trainers unless class has <4 participants) |
| Length and distribution of training: | (e.g., ChYMH Assessor Training will take two days back-to-back plus a one-day “clinical utility” session occurring 2 weeks later; Screener Assessor Training will occur over two back-to-back half-day sessions) |
| Platform: | (e.g., Adobe Connect) |
|---|---|
| Trainer and Support Ratio: | (Note: A minimum of 1 trainer to deliver content and 1 trainer/support person to manage technology is recommended) |
| Length and distribution of training: | (e.g., ChYMH Assessor Training will occur over a single week: 5 half-day webinar sessions) |
3. Determine who will deliver Assessor Training:
- In-house trainers – Requires a) Train-the-Trainer training from outside source, or b) in-house development of new curriculum
- External trainers – Requires partnership with another organization
C. Add literacy training to your plan
Who else needs to have practical knowledge of the tools and how to use the results? Identify participants for Literacy Training.
| Participants: | Estimated number of participants: | |
|---|---|---|
| Delivery logistics: | In-person Web-based | |
| Trainer details: | In-house External | |
| Class size estimate: | ||
| Trainer Ratio: |
D. Determine timelines
1. Using the information documented in Steps A, B and C, determine how many training sessions are needed for each tool by dividing the number of participants needed by the standards for class size (Tip: it can be useful to take the midpoint between the class size minimum and maximum as this will allow you to scale class size up or down depending on how much time you have [see below]).
If any overlap in assessor pool was noted in Step A, consider your options for reducing redundancy. You may wish to incorporate a “top-up training” approach:
- Assessors who will be using both the ChYMH and Screener can attend a full ChYMH Assessor Training and then a shorter session that focuses only on what is different in the Screener.
- Assessors who will be using both the ChYMH and ChYMH-DD can do the same with a ChYMH-DD “Top-Up” that focuses on population-specific factors.
| Approximate number of sessions required | |
|---|---|
| ChYMH: | |
| ChYMH-S: | |
| ChYMH-DD: | |
| “Top-Up” sessions: | (Include type of session) |
| Literacy: |
2. Use a training calendar to plot these sessions between the “Go Live!” date and your desired training launch date, and make adjustments as needed. Choose a person who can coordinate training, and update the Training Calendar.
- Training Coordinator:
Appendix h: training calendar sample
This sample template can be used in conjunction with your training plan. The training calendar secures resources and identifies contacts for each training session. This can be particularly helpful in predicting the resources that you will need and ensuring alignment with other initiatives.
| Type of training | Dates for training | Attendees | Class size | Trainers booked *lead trainer (organization) | Location of training | Training contact for registration | Training contact for materials |
|---|---|---|---|---|---|---|---|
| ChYMH (winter) | January 5th/6th February 10th | New hires | 1-16 max | Becky Red* (Organization A) Beth Green (Organization A) | Organization A | Cathy White | Julie Black |
| ChYMH (spring) | April 5th/6th May 10th | New hires, supervisors | 1-16 max | Mike Blue* (Organization B) Mandy Pink (Organization A) | Organization B | Cathy White | Julie Black |
| ChYMH (fall) | October 5th/6th November 10th | New hires | 1-16 max | Mike Blue* (Organization B) Mandy Pink (Organization A) | Organization C | Cathy White | Julie Black |
| ChYMH for day treatment | August 28th/29th October 17th | Current day treatment team | 1-16 max | Mike Blue* (Organization B) Mandy Pink (Organization A) | Organization C | Cathy White | Julie Black |
| Screener (spring) | April 7th | New hires | 1-16 max | Mike Blue* (Organization B) Mandy Pink (Organization B) | Organization B | Cathy White | Julie Black |
| Screener (fall) | November 7th | 1-16 max | Mike Blue* (Organization B) Mandy Pink (Organization B) | Organization B | Cathy White | Julie Black | |
| Literacy training (spring) | March 25th from 10-12 | New hires, supervisors | 5-16 max | Becky Red* (Organization A) Beth Green (Organization A) | Organization A | Cathy White | Julie Black |
| Literacy training (fall) | October 25th from 10-12 | New hires, supervisors | 5-16 max | Becky Red* (Organization A) Beth Green (Organization A) | Organization A | Cathy White | Julie Black |
Appendix i: resource for navigating “sticky issues” in assessor training
As with any training, there are some common pitfalls in Assessor Training. Be ready for these by reviewing the following support strategies. Review and use your Communication Plan to ensure that messages are consistent.
Sticky issue #1: Participants may have a mental model of assessments that does not match how the ChYMH Suite tools are constructed.
This might look like:
- Discomfort with information being collected in a semi-structured interview rather than a questionnaire.
- Discomfort with the way that information is coded as a summary statement (the “what’s happening”) rather than immediately clinically scored (“how severe is it”). Or, discomfort with information being collected in codes instead of a narrative.
- Difficulty adapting to results that summarize risk and need rather than results that focus on diagnostic information.
You can be ready to support by:
- Expecting that people with scripted assessment experience may want to fall back on those trusted skills and will need support to shift to a conversational interviewing approach.
- Recognizing that mental health workers may be intimidated by summarizing need in ‘one code’ or with ‘one statement’, knowing the complexity of the young people they support.
- Helping by reminding learners that:
- multiple aspects of need are coded elsewhere in the tool, creating a fuller picture, and
- note sections can be used to add context.
- Emphasizing understanding children/ youth holistically, and discussing how to focus intervention when multiple areas of need are identified.
Sticky issue #2: Participants may make assumptions about changes to roles, programs or processes. If misinformation is not dispelled, this can create a significant barrier to learning.
This might look like:
- Learners aren’t clear on why they are becoming assessors, and they don’t understand how the results will be used in their role.
- Tool learning is getting derailed by questions about changes to processes or duties.
You can be ready to support by:
- Being prepared to discuss how being an assessor will (or will not) change their work. Show how choices were made, and allow time for the message to be understood.
- Having a plan for managing ‘out of scope’ conversations such as a leadership contact to address any ‘parked’ questions.
Sticky issue #3: Participants may become overly focused on coding rather than clinical applications
This might look like:
- Participants are overwhelmed by learning the process of coding and conclude the assessments are ‘only for data’.
You can be ready to support by:
- Reassuring participants that the information they collect will be valued and used to support children, youth, and families.
- Emphasizing that the assessor learning curve does begin with coding fundamentals but leads to clinically helpful outcomes.
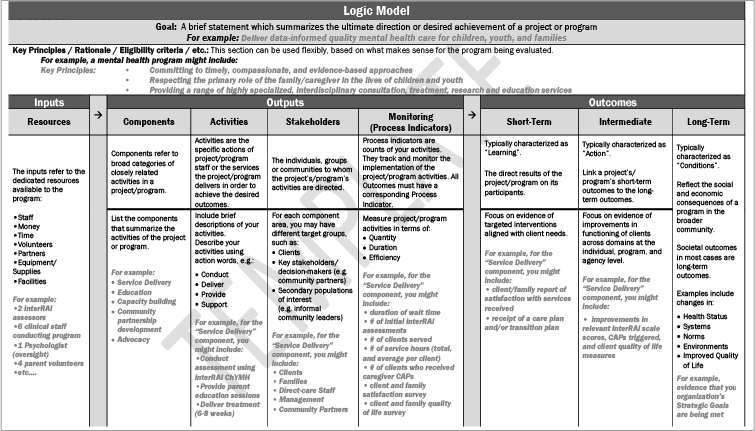
Appendix j: sample logic model for program evaluation using ChYMH
Appendix k: evaluation planning template
The Evaluation Planning Template expands upon the outcomes and indicators identified in your Implementation Logic Model. Use this template to identify how these indicators will be measured. Add as many rows as needed for additional outcomes and evaluation questions.
| Outcome | Evaluation question | Indicator(s) | Target(s) |
|---|---|---|---|
| Outcome 1 For example: Enhanced use of data to inform clinical and service decision-making | Are clinical staff using ChYMH data to inform care planning? | # of programs with ChYMH assessment components embedded into clinical procedures (e.g. reports, processes) | Clinical staff |
| Are clinical staff using Screener+ data to inform triage decisions? | % of intake staff responding positively to the question, “My team uses Screener+ data to make triage decisions?” | Clinical staff (intake department) | |
| Outcome 2 | |||
| Outcome 3 | |||
| Outcome 4 | |||
| Outcome 5 |
Appendix l: data collection and management template
Once your Evaluation and Monitoring Plan is complete, use this template to plan how data will be collected, stored, and analyzed. Add as many rows as needed for additional data sources.
| Data Source | Timeline/ Frequency of measurement | Person(s) responsible | Data management system | Timeline/ Frequency of analysis |
|---|---|---|---|---|
| Data Source 1 For example: Staff satisfaction and use survey | Initial survey: 3 months post-Go Live date Follow-up survey: 9 months post-Go Live date | Implementation Team Quality Assurance Lead | Survey Monkey/Excel dataset | Immediately following each data collection period |
| Data Source 2 | ||||
| Data Source 3 | ||||
| Data Source 4 | ||||
| Data Source 5 |
Appendix m: assessor competency checklist
The Assessor Competency Checklist focuses on competencies related to interviewing clients and their caregivers using ChYMH Suite assessments. This resource may be helpful at several points of learning such as when shadowing a skilled assessor, when meeting with clinical supervisors, or when collaboratively planning to support an assessor who is struggling.
| The assessor… | How this is helpful: | How to enhance skill in this area: |
|---|---|---|
| Knows the items, sections, and similar groupings in the tool |
|
|
| Connects similar items across the tool |
|
|
| Creates a plan for items that are more challenging |
|
|
| Adjusts language in the interview according to the audience |
|
|
| Issue: The assessor is taking a very long time to complete assessments. | |
|---|---|
Gather information to understand how they’re working with the tool(s)
| Possible support approaches
|
| Issue: The assessor is struggling to collect information about all the items in the tool. | |
|---|---|
Consider:
| Possible approaches to support:
|
| Issue: The assessor is struggling to manage the interview process, including incorporating multiple sources. | |
|---|---|
Consider:
| Possible approaches to support:
|
Appendix m: trainer competency checklist
The Trainer Competency Checklist focuses on competencies related to delivering ChYMH Suite training. This resource may be helpful at several points of learning such as when shadowing a skilled trainer, preparing/reflecting on a training, or when collaboratively planning to support a trainer who is struggling.
| The trainer… | How this is helpful: | How to enhance skill in this area: |
|---|---|---|
| Prepares materials and technology ahead of time |
|
|
| Establishes shared expectations with learners |
|
|
| Monitors group energy levels and takes breaks or adapts approach as needed Adjusts language in the interview according to the audience Leads group discussions successfully, drawing on learner experience and promoting balanced participation Acknowledges that asking questions may be difficult, but assures safety and support in doing so |
|
|
| Assesses comprehension formally (such as using evaluation handouts) and informally (such as verbal check-ins, circulating) throughout the training |
|
|
| Works collaboratively with co-trainers |
|
|
| The trainer… | How this is helpful: | How to enhance skill in this area: |
|---|---|---|
| Prompts assessors to consider ‘what would they do’ with the outputs Uses examples that are relatable to the participants Brings relevant case examples into the active learning activities Incorporates documents that are used at your organization into the training |
|
|
| Describes the importance of evidence-informed decision-making (at your organization and in the sector) |
|
|
| Issue: The trainer is not completing training in the recommended time. | |
|---|---|
Consider
| Possible support approaches
|
| Issue: The trainer is completing training in well under the recommended time. | |
|---|---|
Consider:
| Possible approaches to support:
|
| Issue: The trainer is struggling to manage classroom behaviour. | |
|---|---|
Consider:
| Possible approaches to support:
|
| Issue: The trainer is not able to describe how to apply the results, or struggles to create relevant examples to support activities or questions. | |
|---|---|
Consider:
| Possible approaches to support:
|
Appendix m: clinical staff competency checklist
The Clinical Staff Competency Checklist focuses on competencies related to understanding and using the ChYMH Suite results. These are core competencies that apply to all clinical staff who work on teams or in programs where the ChYMH Suite is used, including assessors and trainers.
| The individual clinical staff member… | How this is helpful: | How to enhance skill in this area: |
|---|---|---|
| Knows the scales/can identify scales best for shorter-term measurement Understands Collaborative Action Plans (CAPs) and how they can be used by clinical staff Uses results to back up clinical formulation or referrals Sets measurable goals with families using the scales or CAPs Uses and refers to scales and CAPs when planning intervention strategies Refers to scales and CAPs in documentation and in conversations with families |
|
|
| The individual clinical staff member… | How this is helpful: | How to enhance skill in this area: |
|---|---|---|
| Knows the outputs (scales, screening algorithms) and how they map on to the tool Refers to scales and screening algorithms in documentation and in conversations with families Uses results to back up triage, service determination, and referral decisions |
|
|
| Issue: It is not clear if/how the results are incorporated into work with the young person or their family. | |
|---|---|
Consider
| Possible support approaches
|
| Issue: The individual is resistant to using ChYMH Suite results to support clinical decision-making. | |
|---|---|
Consider
| Possible support approaches
|
| Issue: The individual struggles with understanding how to use the results to support clinical work. | |
|---|---|
Consider
| Possible support approaches
|