Module 2 – implementation phase 2: planning
Module objectives
The purpose of this module is to guide implementers through the activities needed to ensure that a successful ChYMH Suite launch can be supported. With this module, you will:
- Develop a plan for how the tools will be used in your organization.
- Develop a cohesive leadership approach to supporting implementation.
- Learn some common pitfalls in ChYMH Suite implementation and develop a risk management plan.
- Learn about the importance of open communication and develop a Communication Plan.
- Explore ChYMH Suite training options and create a training plan that fits your organization’s needs.
- Learn how to successfully launch ChYMH Suite training.
- Develop a plan for monitoring and evaluating your implementation effort.
2.1 Identifying how the ChYMH suite will be used in practice
The primary purpose of the interRAI ChYMH Suite is to support clinical assessment and client care decisions. The tools also have the capacity to support other core processes, including program evaluation, resource allocation, and accountability requirements (such as data requests from funders or board of directors). The following is a guide to mapping how the interRAI ChYMH Suite can be used in your organization.
In Module 1 you identified which ChYMH Suite assessments and which programs/services will be the focus of the implementation effort. You also spent some time identifying your organization’s goals. The next step is reviewing your current processes to determine how to make tool use work best for your organization, and what will need to change to support the new practices.
ChYMH assessment types
Before you can map the ChYMH Suite tools to your organization’s processes, you need to know your options for variations based on where the client is in their service path.
The ChYMH Screener is designed as a pre-service screener only, although some organizations have used it as a post-service assessment. See www.interRAI.org for recommended uses.
The comprehensive assessments – the ChYMH and the ChYMH-DD – have been used for varying service purposes. Availability of the versions outlined below is not dictated by interRAI and is dependent on your software solution.
| Service | Description |
|---|---|
| Initial | A full ChYMH/ChYMH-DD assessment, used at intake or beginning of service. |
| Subsequent | A full ChYMH/ChYMH-DD assessment, used at one or more midpoints in service. |
| Monitoring | A short, focused, individualized assessment that includes only the items needed to evaluate current status on one or more outcome measures. Has been used only with a prerequisite that a full ChYMH/ChYMH-DD assessment is completed first. |
| Discharge | A full ChYMH/ChYMH-DD assessment, used at the end of service. |
| Discharge Tracking Only | A ChYMH/ChYMH-DD assessment that has been shorted only to essential information for tracking end of service. This assessment type is only appropriate for clients who drop out of service and cannot be assessed for clinical progress. |
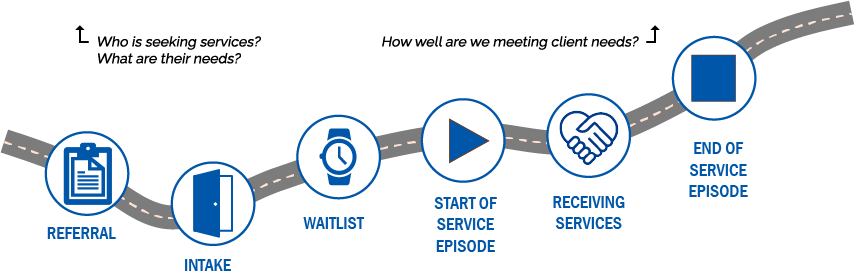
How the ChYMH suite provides useful data along the service path
This graphic provides an example* overview of the ways that ChYMH Suite data can support service delivery and organizational decision-making at key points along the service path. As you begin to plan where in the service path the tools will be used in your organization, consider how you want to leverage ChYMH Suite data to support your clients, staff, and programs.
Screening: ChYMH-Screener
- Triage & prioritization
- Service determination
- Profile of client needs (focused)
Baseline: ChYMH/DD Assessment
- Service planning
- Baseline clinical status
- Profile of client needs (comprehensive)
Monitoring: ChYMH/DD Monitoring Assessments
- Monitoring of client progress and treatment efficacy
- Targeted; based on client’s unique needs
End of Service: ChYMH/DD Assessment
- Post-intervention clinical status
Tool use mapping
Mapping is a multi-step process that requires those who have intimate knowledge about your organization’s current processes to be at the table.
Start where you are. Map out your current processes and think about where the assessment versions (initial, subsequent, monitoring, discharge) naturally fit. Then consider who will be assessors and how completion of the tools may impact clinical timelines. Consider what information you need at what time: for example, what do you need to know for treatment planning, for ongoing service planning, and as the young people leave your services? Factor this in to how and when you will use the tools.
Be realistic and allow for some flexibility during the initial few months. Let staff know that you appreciate their feedback and are open to discussions around where the tools would best fit within specific programs to bring the most benefit to both staff and clients.
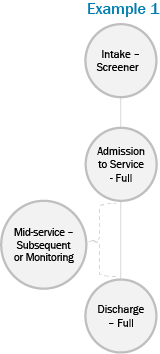
In Example 1 the tools are mapped so that the Screener supports triage, a full ChYMH/ChYMH-DD assessment informs planning, monitoring or subsequent full assessments inform progress evaluation, and pre/post comparisons can be made to evaluate treatment success.
This might work well for an organization with complex clientele, longer-term services, and where evaluation is a priority.
In Example 2 the tools are mapped so that they provide the data needed for initial planning and for pre/post evaluation.
The first option might be best at an organization with more complex clients and treatment programs, and the second might be best at an organization with fewer, less complex treatment programs.

In Example 3, the assessment is used for an initial assessment of needs only. This might be chosen by an organization that delivers very brief services and where pre/post evaluation is not a priority.
Worksheet: guiding questions to support mapping
In answering these questions, consider gathering feedback from program managers or direct care staff to determine what processes are realistic and likely to succeed.
1. What kind of information do you need? Where in the service journey do you need it?
For example: Are you primarily interested in an overview of current needs and risks at intake? Do you also need outcome information at the end of service? What about during?
2. What assessment documents, scales, checklists are currently in use? Can any current tools or processes be replaced with the new tools/practices to avoid redundancies and reduce burden on staff and clients?
For example: Does your organization use other standardized tools? What about “homegrown” assessments? Can existing tools, including forms that collect narrative information, be replaced?
3. What problems or frustrations exist in the current workflow? Does the ChYMH Suite implementation offer an opportunity to address current issues?
For example: Are there bottlenecks, duplications, or service quality issues?
4. What are your current clinical processes?
Map out service processes, noting when and how information is gathered, used, and documented. Are there times when information is gathered but not used?
5. How will your information management processes need to change?
For example: Where will completed assessments be stored? How will completed assessments be shared externally? Do appropriate sharing and consent mechanisms already exist, or will changes be needed?
6. What guidelines will be put in place regarding timelines?
Consider:
- How often will full assessments be completed? How old can an assessment be before it is considered “out of date”?
- How frequently will monitoring or subsequent assessments be completed?
- Will these standards be the same across all programs?
7. Who will administer the ChYMH suite assessments? What are the resourcing implications?
Consider what can stay the same and what will need to change, including:
- Which disciplines and roles will be ChYMH Suite assessors?
- Do the staff who currently administer assessments have the clinical experience to administer ChYMH Suite tools, or will this responsibility need to be shifted to more qualified staff?
- Are adequate supervision practices in place?
- What additional resources (e.g., time, technology) will be needed?
8. Who do you know that has successfully adopted the ChYMH Suite into clinical practice? Can you learn from their mapping experience?
Consider organizations with similar services or workflow.
2.2 Leadership and ChYMH suite implementation
To successfully implement a change in any organization the managers and supervisors must be “on board”. Employees look to managers and supervisors not just for direct messaging but also to determine how supportive of the change they should be.
If a manager or supervisor only passively supports – or is resistant to – the change effort, employees will likely adopt the same attitude.
Leaders’ support for the change must be both active and observable by the rest of the organization.
Managers and supervisors are a lynchpin in the success of a change initiative. In times of change, those who lead the teams impacted by the change can be both a great ally and a real obstacle for change leaders. (Prosci, n.d.)
Steps to engaging leaders to support ChYMH suite implementation

Get everyone “on board”
Getting leaders on board with the change initiative is one of the first steps in successfully implementing the interRAI ChYMH Suite. Support from leaders will allow every step in the implementation process to be met with greater levels of enthusiasm and motivation.

Make sure leaders are sending a strong message
Implementation of the interRAI ChYMH Suite is a significant undertaking. Leadership needs to voice a strong message that outlines the urgency and key benefits of using the tools as well as risks associated with an unsuccessful launch. To successfully implement the interRAI ChYMH Suite this message must be heard at all levels of the organization.

Watch out for individuals who are resistant to the change
Organizations who have resistance at the management level – particularly from those who directly supervise the clinical teams – are far less likely to experience successful implementation and integration of the interRAI ChYMH Suite into routine practice. This results in assessors showing less fidelity to the tools, leading to the organization having inconsistent or poor data for client support.

Get everyone “on board”
Getting leaders on board with the change initiative is one of the first steps in successfully implementing the interRAI ChYMH Suite. Support from leaders will allow every step in the implementation process to be met with greater levels of enthusiasm and motivation.

Make sure leaders are sending a strong message
Implementation of the interRAI ChYMH Suite is a significant undertaking. Leadership needs to voice a strong message that outlines the urgency and key benefits of using the tools as well as risks associated with an unsuccessful launch. To successfully implement the interRAI ChYMH Suite this message must be heard at all levels of the organization.

Watch out for individuals who are resistant to the change
Organizations who have resistance at the management level – particularly from those who directly supervise the clinical teams – are far less likely to experience successful implementation and integration of the interRAI ChYMH Suite into routine practice. This results in assessors showing less fidelity to the tools, leading to the organization having inconsistent or poor data for client support.
Self-assessment: Is your leadership team ready to support staff through ChYMH suite implementation?
This self-assessment contains some prompts to get you thinking about your organization’s leadership team and whether it is ready to provide strong, consistent, and united support to staff through the ChYMH Suite implementation process.
This is a crucial step – if the answer to any of these considerations is “no”, managers and supervisors will not have sufficient knowledge, tools, skills, or motivation to aid in implementing the change. Remember that managers and supervisors will be the ones that continue the coaching role after training has been completed. It is their responsibility to support staff in use of the assessments on a day-to-day basis. Therefore, their commitment to the implementation of the interRAI ChYMH Suite is essential. As you review the prompts, make note of your answers and thoughts.
Tips for leaders
Leading as a Team
- Remember that ChYMH Suite implementation will require leadership support from multiple areas of the organization, all with different perspectives and values. Pay attention to your own values and biases, and honour others’ as well.
- Be proactive! Use the wisdom of the team to identify and remove obstacles before they become an issue.
- Remember that leaders cannot lead an implementation that they don’t understand . Take responsibility for learning about the ChYMH Suite assessments and how these tools can be integrated into clinical practice for best outcomes.
- Make supporting staff a top priority. There are many operational benefits to using the ChYMH suite that leadership may be inclined to focus on. However, it’s important to remember that without a focus on valuing the clinical benefits of the tools clinical staff will lose interest and data quality will suffer.
- Remember that implementation is a multi-year process therefore leadership commitment must be as well. Be consistent and deliberate in your ongoing support of the new practice.
- Remember that change requires change! Challenge outdated assumptions and don’t be afraid to push back against the tendency to do things “they way they’ve always been done”.
Communicating with Action
Consider how the following leadership behaviours can communicate that ChYMH Suite implementation is an organizational priority:
- Focus: What a leader notices, comments made, questions asked, and how agendas are set all communicate priorities to staff.
- Reaction to Crises: How leaders define what is and what is not a crisis reveals underlying norms and values.
- Resource Allocation: Dedication of time, money, and staff reveals where priorities lie.
- Role Modeling: Role modeling, teaching, and coaching provide a visible method for communicating values to others.
- Recruitment: The criteria for recruitment, selection, and promotion is a powerful indicator of where the organization’s priorities lie.
- Reward and Status: Staff learn from experiences with feedback, praise, and discussion. Which behaviours and actions are rewarded or disciplined is a clearer message than what is said.
Leadership activities planning
CPRI has developed a planning worksheet to support leaders as they in turn support their organizations though the implementation process. This worksheet can assist with planning and managing some of the common tasks for leaders of a ChYMH Suite implementation effort.
The activities in the Leadership Activities Planning worksheet are grouped into three categories implementation science confirms are crucial for successful implementation:

Administrative Support
Leaders must facilitate the implementation effort by proactively finding and addressing challenges, creating and adjusting policies and procedures, and creating effective communication and feedback systems.

Systems Intervention
Systems intervention is required when barriers exist outside of the immediate control of the organization’s leadership.

Data & Decision Support
Leaders need to create effective decision-support systems based on quality data to support informed decision-making.
As you consider Leadership Activities, consider which approaches can support effective leadership. In some instances, a blend of both technical and adaptative leadership will be required.

Technical
Technical leadership is needed when tasks and challenges are routine and straightforward. Technical leadership involves applying solutions and steps that are familiar.

Adaptive
Adaptive leadership is needed when tasks and challenges are complex and no clear solution exists. Adaptive leadership involves collaboratively defining the problem and mobilizing staff to create possible solutions.
2.3 Risk management
Risk management is an important step in the Planning phase of implementation. CPRI created a Risk Management Planning tool to aid in identifying and mitigating risks related to implementing the ChYMH Suite. This tool will help you consider potential risks, estimate their significance, and determine what an appropriate plan to address the risks might be.
Some common areas of risk in ChYMH Suite implementation are:
- Inadequate support for new assessors as they learn to complete assessments (for example, not allowing extra time for assessment appointments, or not allowing assessors to work in pairs initially)
- Insufficient access to technology (for example, enough computers, access to printers, consistent internet access)
- Not having a clear and multifaceted communication plan throughout the implementation process
- Not having a clear path for staff to ask questions and express concerns, or not having a mechanism for responding to feedback
- Not having a plan in place for responding to “naysayers”
- Not having champions available to support staff and answer questions
Consider the following aspects of risk review as you work through the Risk Management Planning worksheet:

Accept
There is always some risk. How likely is the risk? Is the risk acceptable within the context of the potential opportunities gained?

Control
What additional actions, processes, or procedures could minimize the impact, severity, or likelihood of a risk occurring. A caution: More rules do not necessarily translate to better control. It is better to consider the root causes of the risk and implement initiatives that align with the organization’s goals than to rely on rules and processes.

Adjust
Can a practice be adjusted to eliminate or reduce risk in a way that does not impact fidelity to core components of interRAI tools and reducing the validity and usefulness of the instruments (see Module 1).

Watch
Whatever management strategy is chosen for an identified risk, it is important to continue to monitor for changes that can affect the nature or impact of a risk – it may be that as situations change, so should your risk management strategy.

Accept
There is always some risk. How likely is the risk? Is the risk acceptable within the context of the potential opportunities gained?

Control
What additional actions, processes, or procedures could minimize the impact, severity, or likelihood of a risk occurring. A caution: More rules do not necessarily translate to better control. It is better to consider the root causes of the risk and implement initiatives that align with the organization’s goals than to rely on rules and processes.

Adjust
Can a practice be adjusted to eliminate or reduce risk in a way that does not impact fidelity to core components of interRAI tools and reducing the validity and usefulness of the instruments (see Module 1).

Watch
Whatever management strategy is chosen for an identified risk, it is important to continue to monitor for changes that can affect the nature or impact of a risk – it may be that as situations change, so should your risk management strategy.
2.4 Communication planning
Communication is one of the most important but challenging elements to get right when implementing the ChYMH Suite. Communicating often, to everyone, and in as many modes as possible is one of the most effective strategies to build buy-in for the implementation effort. Doing so helps build momentum and dissuade negativity or anxiety about the upcoming change.
Communicating well takes significant time and effort so planning is important. As you plan your efforts, keep the following principles in mind:
- Manage style and content of communication . Leaders and managers should pay attention to their tone and be honest and open in their communications. Consider your audience – start by addressing what is most important to them.
- Disseminate information regularly and clearly. It is important to provide regular updates even when there is “no news”. Roles, tasks, responsibilities, and procedures need to be clearly defined.
- Ask for input . Use communication as a vehicle for participation. Active participation can deactivate rumours and allows for a healthy work environment where employees feel their concerns are being addressed.
- Motivate! Encourage risk-taking, pay compliments, and single individuals out for praise where appropriate. Be careful not to ignore reality in favour of being positive, though. A pattern of unfulfilled promises undermines leadership and management credibility and can lead to perceptions of injustice, misrepresentation, and violations of trust.
| Key Feature | Rationale |
|---|---|
| Why do we need a new assessment tool, and why the ChYMH (or ChYMH-DD, or ChYMH Screener)? | This should be part of your vision statement and an idea that you repeat over and over, every chance you get. |
| Who is going to do this? How does this fit with our current process? | It is important to tackle these questions before training. Ensure your soon-to-be assessors know the answers to these questions to reduce anxiety. Be transparent and share how and when you see the assessment fitting in their process. |
| How will we learn to do this? When will we learn to do this? | Share information about the training plan early to allay anxiety about how people will learn the specifics of the assessment. No one likes a “surprise” 3-day training! |
| What do we tell our clients/ families? | Create a plan for introducing the new assessment to families. Ideally, this plan would be co-created with clinical staff. Share the plan widely and discuss who will do the communicating to the families well ahead of launching the tools. |
| Who do I talk to if I have questions or concerns? | Ensure that staff know who to contact and create a safe environment for feedback by offering multiple ways to express questions or concerns, such as a drop box, confidential email, or monthly meeting. |
Building buy-in at your organization
As with any major organizational change, creating buy-in for the ChYMH Suite will take time and patience, and should be an integral part of planning from the outset. In CPRI’s experience, these are some of your best tools and approaches for building buy-in at your organization:
Facilitate engagement with key stakeholders (such as clinical and program leads) to solicit ideas and feedback on how to best integrate the tools into clinical practice.
Buy-in involves all levels of the organization. Remember to collect opinions from all groups/programs when assessing current buy-in.
Build credibility by being prepared to answer questions knowledgeably concerning the tools and how they will benefit your organization.
Work with dissenters early in the process.
When encountering resistance, it is important to identify and understand people’s underlying emotions and concerns.
True buy-in requires at least some level of co-creation. Invite staff and other stakeholders into discussions about changes to practices and processes. This will allow everyone to feel more invested in the outcome.
Create and maintain motivation by focusing on the benefits of implementation. For example, communicate the urgent need to demonstrate data-driven services and use of evidence-based strategies.
Highlight how the tools will be beneficial for both the organization and for clients. Consider using anecdotal stories to do this, as these can be both compelling and memorable.
Take the time to understand the motivations of your stakeholders. What do they see as potential impacts of the implementation, both positive and negative? How are these opinions impacting buy-in?
Make supporters visible.
If managers, opinion leaders, or peers support the implementation, employees are more likely to see its value.
CPRI’s 3-step process for communication planning
An important step in the earliest stages of starting an interRAI implementation effort is completing the Readiness Self-Assessment, which can be found on the next page.
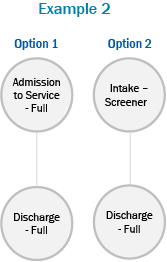
 Step 1: Identify your stakeholders
Step 1: Identify your stakeholders
A stakeholder map of common direct and indirect stakeholders in ChYMH Suite implementation is provided below. Does this reflect the stakeholders for your implementation? Do any need to be added or removed?
 Step 2: Consider stakeholders’ unique needs
Step 2: Consider stakeholders’ unique needs
To plan communication with your stakeholders, take their individual needs into account. Consider the following questions for each stakeholder group individually:
| Who | Which stakeholder do you need to communicate with? | For example, staff and board members |
| Context | What does this stakeholder group already know? | For example, leadership is planning to adopt a new standardized assessment system. |
| What | What is the purpose of your communication? What are the messages you want to share? | For example, if the purpose is to keep staff aware of the implementation progress, the messages to share might include a status update and timelines for upcoming milestones |
| How | Who will prepare and deliver the communications? Through what means? What resources are required? | For example, the Implementation Team will prepare the communications and leadership will send via all staff emails and discuss at upcoming staff meetings. |
 Step 3: Prepare your Communication Plan
Step 3: Prepare your Communication Plan
To access the Communication Plan template, see Appendix G.
2.5 Training planning
Creating a training plan for your organization will serve as the foundation for both initial assessor training and ongoing training needs.
Keep in mind that:
- Initial Assessor Training will look very different compared to ongoing training, and both must be addressed to create a solid training plan for your organization.
- Ideally, training planning should occur only after tool use mapping, communication and risk planning has been completed.
- Training should be approached with intention – training large groups of staff with the intent to “figure out the details later” does not achieve positive results.
- The four types of training that you will need to consider are:
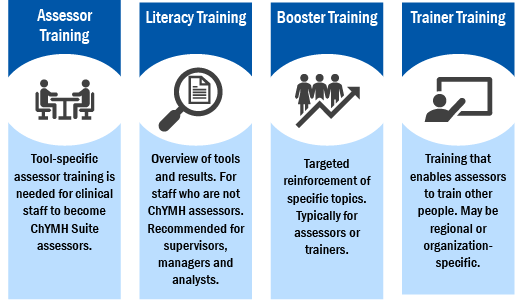
About the ChYMH suite curriculum:
To support successful and widespread use of the ChYMH Suite in Ontario, CPRI developed a comprehensive training curriculum for the ChYMH, ChYMH-DD, and ChYMH-S that is used to support ChYMH Suite learning needs across the province. Whether you use CPRI’s training curriculum or develop your own, be aware that:
- The most important factor in successful ChYMH Suite training is a strong focus on how to use the tools in clinical practice, embedded and emphasized throughout the entire training session.
- Key components of assessor learning needs are: how to use the manual to code assessment items, how to conduct a semi-structured interview, and how to read, understand, and use the assessment results in clinical practice.
- Literacy Training focuses solely on how to read, understand, and use the assessment results in clinical practice.
- Booster Training sessions should be a regular part of the training plan, and can be tailored to the skill-building needs of your organization.
- Within CPRI’s curriculum, trainers must complete assessor training (for each tool that they are going to train) prior to attending Train-the-Trainer training.
Setting yourself up for training success – initial training
Planning for initial training
During the initial training phase, the priority is preparing staff for the launch of tool use at your organization. Assessor Training and Literacy Training are the focus.
Identify your training timeline
- Decide the date you want assessments to start and work backwards.
- Do not start training until mapping is complete. Make sure that participants have a general idea how assessments will be used in your organization, so that they can make sense of how they will be using their new skills as they learn them.
Determine the number of assessors that are needed.
To estimate, consider:
- How frequently assessments will be completed on clients.
- Assessors should be completing at least 3 assessments per month in order to develop and maintain skills.
If you are implementing more than one ChYMH suite assessment, determine:
- Will the same assessors be trained to administer multiple types of assessments, or will there be a different assessor pool for each?
- Is there an opportunity to streamline training and eliminate redundancies? For example, an assessor cohort that takes a combined ChYMH/ChYMH Screener Assessor Training, and a Literacy Training session that teaches non-assessor clinical staff how to use both tools for clinical decision-making.
Determine a class size minimum and maximum.
This will allow you to predict how many training sessions will be needed and determine how resources can be used efficiently. Consider:
- Training type: Literacy Training can have a higher participant-to-trainer ratio, whereas Assessor Training requires a lower participant-to-trainer ratio that allows more hands-on support.
- Experience of trainers: For Assessor Training, a maximum of between 8-16 learners per class is recommended, with the range dependent on trainer experience. Literacy Training sessions can accommodate larger groups such as 20-25 participants.
- Availability of trainers: It is recommended to have two trainers facilitate Assessor Training . CPRI’s guideline is that two trainers are needed when a) class size is greater than 4 or b) trainers are first learning, regardless of class size. Literacy Training can be delivered by one trainer.
Consider time resources and other pressures:
- Length of time for assessors to attend a training session and whether backfill will be needed. In CPRI’s curriculum, Literacy Training takes a half day, Screener Assessor Training takes a full day, and ChYMH/ChYMH-DD Assessor Training takes 3 days.
- Other competing priorities, for example, are there other training initiatives that are taking staff time?
Setting yourself up for training success – ongoing training
Planning for ongoing training
Once the initial training phase is complete, training needs shift significantly. Ongoing training may include smaller classes or even one-to-one sessions when needed. Assessor Training and Literacy Training will primarily be needed to offset staff turnover, and Booster Training will become a very important part of your training plan.
Ongoing assessor and literacy training
- Consider how much staff turnover your organization typically experiences. If turnover is moderate to high, consider scheduling regular (e.g., twice-yearly) Assessor Training and Literacy Training sessions.
- To avoid making inconsistent and potentially costly decisions, make a guideline to outline a class minimum and a plan for meeting assessment needs if the minimum is not met.
- Select a Training Coordinator who can support ongoing training by:
- Managing booking and other logistics
- Securing materials needed for training
- Acting as a contact for cancellations/confirming attendance
- Assessing your organization’s resources and training needs
- Keep the following guidelines in mind:
- For smaller classes (fewer than 4 participants) a single trainer will usually suffice.
- Remote learning often requires a second facilitator to manage chat boxes, off-line questions, and any technology issues.
- No matter how small the class is, it is important to still follow the curriculum – even for a one-on-one session. In our experience, drifting away from the curriculum is one of the greatest threats to assessment quality and implementation sustainability.
Booster training
- Incorporating regularly scheduled booster sessions for assessors and other clinical staff is one of the best ways to support staff as they develop competence and comfort with using ChYMH Suite tools.
- Booster sessions can take many different forms, such Lunch-and-Learn gatherings, self-guided learning modules, trainer-led virtual training sessions, and interactive newsletter features.
- When designing booster sessions, consider the following:
- Think about the evolution of an assessor: a new assessor usually needs support first with coding, then with interviewing, and then reading and using assessment results.
- Be strategic. Do an environmental scan, and choose topics that are relevant to your staff and will encourage participation.
- Be playful. Consider doing fun themes such as “
- Collaborative Action Plans, or CAP
- Be predictable. Assessors will know where to look for information if you stick to a consistent look or schedule. This will also be helpful in the future, should you need to announce any changes or updates to your processes.
Developing a training team
Building a training team is a critical element is sustaining a successful implementation. Your training team will prepare new staff, and ensure existing staff continue to use the tools accurately and consistently. This section will provide guidance around decisions to make.
Decisions about your organizations training needs are dependent on resource availability. Remember to consider opportunities outside your organization. Consider natural partnerships such as a neighbouring organization also using ChYMH Suite tools where there is an opportunity to discuss sharing resources. Whether you choose your own path, or walk with another, you can also shift as your needs change or develop.
Where does your organization fall along the continuum of training needs below?
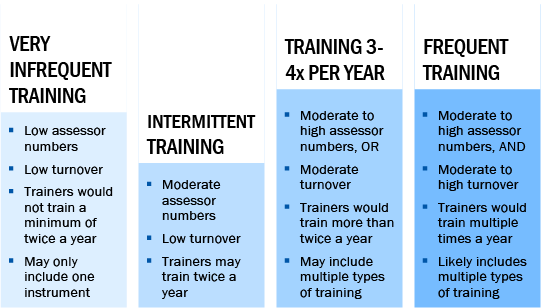
In the first two examples, it may not make sense to have organization-specific trainers, as they would not train enough to maintain skills. Consider partnering with another organization to create more frequent training opportunities together.
In the third and fourth examples it may be suitable to have your own training team comprised of several trainers from your organization, or to collaborate with other organizations to create a regional training team.
Benefits of training teams:

Opportunity for more predictable training calendars and fuller classrooms

Greater consistency in training delivery across trainers.

Knits together a community of assessors and trainers by increasing peer-to-peer involvement.

Supports mentoring of newer trainers.

Able to provide insight and advice to the Implementation Team.
Setting up your ChYMH suite training team
Identify your trainers
Trainers are a critical element to overall implementation success and should be selected with intention. Trainers are champions that can inspire, guide, and be an excellent resource to assessors, committees and decision makers.
When selecting trainers, consider:
- Do they have previous training experience? If not, are they interested in developing presentation or facilitation skills?
- Are they enthusiastic about the initiative? Will they be able to maintain an encouraging attitude about the instruments and implementation?
- Do they have clinical experience to draw on to describe relatable instances and illustrate how ChYMH Suite tools will be clinically beneficial?
- Will they be able to create a supportive learning environment? For example, will they be adept at explaining clinical concepts or creating a safe environment for sensitive topics?
- Do they have a history of demonstrating emotional acuity in sensitive situations? For example, are they skilled at managing conflict or helping someone problem-solve through a frustrating situation?
Pull together the team
Whether your organization creates its own in-house training team or joins with others to create a regional training team, start by addressing:
Team roles:
- Membership should include trainers and training coordinators, and may also include others such as management, Information Technology and Quality Assurance representatives.
- A Terms of Reference document or other formal agreement can be used to clarify tasks and duties.
Team responsibilities:
- Defining the parameters for training at your organization/the organizations in the collaborative. This should include classroom parameters (such as class size minimums and maximums, designated lead trainer) and resource parameters (such as time for trainers to prepare, printing of materials, sourcing of training rooms).
- Planning and implementing Booster Training.
- Planning and maintaining communication with the Implementation Team (such as reporting concerns, sharing training evaluation results, sharing successes).
- Communicating important information with the rest of the organization such as celebrating successes, sharing tips in newsletters, open training calendars.
- Supporting assessors by being available to answer questions and listen to ideas.
2.6 Training launch
Launching initial training
For many at your organization, the launch of initial training will be the ‘big event’ when they start to see real change happening. Although it is tempting to rush training, this should always be a well-planned effort that is the end result of careful and detailed implementation work.
Initial training is when there are greater numbers of participants, all learning at the same time. Because this is new ground, there are fewer people with a strong understanding of the details of the implementation. Everyone is learning with a beginner mind.
Preparing for training
- Confirm bookable resources. Trainers will need to reserve the training environment (live or web-based classrooms) and any technological resources needed for training such as laptops or secure training lines
- Clarify roles. Apply the training plan/calendar to indicate who the trainer (or lead trainer if there are multiple trainers) and training coordinator will be.
- Register participants. Trainers will need to gather all the contact information needed prior to the training. This includes confirming any prerequisite training has been completed.
- Prepare materials. Trainers will need to confirm that any training materials are printed, circulated, or otherwise made accessible to participants. This includes the trainers’ own print materials, manuals, and supplies such as white board markers or props.
- Direct participants. Trainers will need to make sure that the participants know how to get to the training. This could include sharing directions, hanging signs or emailing password access to training participants.
- Review the training plan. A review of the curriculum plan prior to training day will help trainers feel confident. If multiple trainers are leading the session, they should connect to review and plan together.
- Prepare for possible “sticky” spots in Assessor Training. A review of the recommendations in Appendix I can help trainers feel confident in their ability to handle common tricky issues if they come up.
On training day
- Set out the welcome mat. Trainers should arrive early to double check the in-person or virtual set-up and to create a welcoming tone for the session.
- Be enthusiastic! Trainers who bring a positive attitude to training make it a wonderful experience for everyone.
- Follow the plan. Guidelines for running activities, facilitating discussions, and timing should be part of the curriculum plan for trainers.
- Take notes. Trainers benefit from recording where they felt challenged, where they had great examples or spots they felt ‘stumped’. Notes can be made by annotating their training guides or using a training journal.
- Park off-track questions. Participants often raise questions that may be out of scope, such as questions about organization processes. These questions are best “parked” and answered outside of the training session. This strategy acknowledges the inquiry but does not interrupt the training.
After the session
- Celebrate and reflect. Trainers can use their notes and training feedback to review their experiences delivering training and identify areas to improve upon for next session.
- Unpark the parking lot. Trainers should gather or summarize questions that were ‘parked’ and either address concerns directly or forward them for follow up.
- Roll up evaluations. Trainers should examine any mid-session comprehension checks and end-of-session evaluations and compile them for overall training evaluation.
- Pass on the congratulations! Consider providing completion certificates to participants to leave learners with a contact for future questions.
- Share impressions. More so than many, trainers are in a position to see the implementation coming to life. Trainers should share their insights with the Implementation Team to help with monitoring and evaluating the implementation as a whole.
- Keep learning. Trainer Communities of Practice can be a great resource for harnessing the experience of other trainers for the benefit of all. Trainers should connect with one another to learn from each other.
2.7 Implementation evaluation and monitoring planning
Evaluating your ChYMH Suite implementation effort is a key part of making sure your implementation is a success. Monitoring and evaluation should be a part of the discussion as each of the implementation planning pieces are completed. Evaluations that are planned and implemented early on produce the most meaningful and useable information. Setting targets for ongoing sharing of evaluation/monitoring results with stakeholders can be an excellent way to ensure that evaluating and adjusting accordingly remains a priority throughout the implementation process.
Why evaluate?

Demonstrates program effectiveness to external and internal stakeholders

Highlights inefficiencies or areas needing further attention

Monitors progress toward goals
Read on for an overview of the steps to creating a comprehensive evaluation plan, and then use the templates provided in the Appendix to create your plan.
Step 1: Develop a logic model.
Clearly outline the implementation activities, how they can be measured or monitored, and what
Step 2: Develop an evaluation and monitoring plan.
Using the Evaluation Planning Template in Appendix K, develop a plan for monitoring process indicators and evaluating outcomes.
Some possible data sources for evaluating outcomes might include:
| Benefit to clients and caregivers |
|
| Benefit to practitioners |
|
| Streamlining services |
|
Step 3: Develop a data management plan.
Using the Data Management Plan Template in Appendix L, make a plan for how the data will be collected and stored. A data management plan is needed for each of the data sources identified in Step 2, and should include information such as data sources and how it will be stored, who will be responsible, and when and how the data will be analyzed.
Mini case scenario #2
The Implementation Team began their mapping exercise by focusing on what information clinical staff need and when they need it. The social work lead suggested that an initial community ChYMH-DD be completed by the social worker at the pre-admission tour for a timely start to needs-based treatment planning. This tour typically takes place within 10 days prior to the admission. This would provide an opportunity for the clinical team to review the assessment, consider the information from results such as Collaborative Action Plans, and develop potential treatment goals to be reviewed with the youth and their caregivers on admission day. After much discussion the team determined that a subsequent inpatient ChYMH-DD will be completed after 6 months. It was suggested that individualized monitoring assessments based on the youth’s treatment goals could be helpful if completed prior to monthly care review meetings. These assessments could be completed by the youth’s primary worker, a direct care staff on the inpatient unit, and would provide consistent data to share with the youth and their caregivers to demonstrate treatment progress. It was further decided that a community-based assessment would be completed within 10 days following the youth’s discharge from inpatient treatment by the social worker on her first home visit.
Organization B provides inpatient treatment services to youth with mental health needs and intellectual disabilities. They have completed the Commitment phase of their interRAI implementation and are actively working on mapping their current service process to determine which tools to use and when assessments will occur. The team is eager to develop both a leadership plan and communication plan to fully support launching the tools in 3 months. They will also develop a training plan that could begin in 2 months.
The team discussed how strong leadership will be necessary to support each stage of implementation. They drafted a leadership plan, identifying contacts and responsibilities for specific areas. This led to a risk management planning discussion. In particular, they focused on eliminating duplication in processes and documentation, and communicating these changes to staff.
Concern was raised about staff buy-in, specifically how to inspire champions and support those with concerns. After reflecting on how past failures to communicate with staff had negatively affected other initiatives, they committed to:
- High-level presentations beginning at the next organization-wide staff meeting
- Ongoing communications via team meetings, emails and direct supervision
- Creating a process for staff input and feedback, and responses to submissions
The last topic was training. Some questioned whether direct care staff should be trained, since backfilling is expensive. The team debated this and eventually concluded that the risk of dividing the clinical team and reducing the pool of trained staff was too great a threat to implementation success. It was decided that all social workers would be trained as assessors, and residential managers would be asked to recommend direct care staff to be trained as well.
Mini case scenario #2 reflection
Guiding questions
- What points along the service path were most important for Organization B during the mapping process? What might the important mapping touchpoints be at your organization? (Consider: Clinically? For data collection?)
- Organization B’s leadership acknowledged past difficulties with communication and resolved to do better with their ChYMH-DD implementation. Are there any challenges in your organization’s history that should be learned from in order to support a successful ChYMH Suite implementation?
- Consider Organization B’s plans for communicating with staff. What other examples of communication processes might help? What would be important to communicate at your organization, and who is best suited to lead this process?
- Organization B is going to involve residential managers to identify who should be trained as assessors. Who would be best suited to identify potential assessors at your organization?
Phase 2 actions checklist
Develop a plan for how ChYMH suite tools will be used.
- Review the different assessment types at www.interRAI.org
- When assessments are completed affects how the data can be used. Review the “How the ChYMH Suite Provides Useful Data Along the Service Path” graphic in section 2.1, and consider how you want to leverage ChYMH Suite data to support your clients, staff, and programs.
- Complete the “Guiding Questions to Support Mapping” worksheet in Appendix C. It may be helpful to refer to the examples in the “How the ChYMH Suite Provides Useful Data Along the Service Path” graphic in section 2.1.
- Identify any changes to the current service path that may be needed in order to align with implementation goals.
Identify and mitigate risks to successful implementation.
- Have a facilitated discussion about risk management with the Implementation Team, including reviewing the common areas of risk in ChYMH Suite implementation that are outlined in section 2.2: “Leadership and ChYMH Suite Implementation”.
- Use the Risk Management Planning Worksheet in Appendix F to identify potential risks for your organization and plan for how to address them.
Prepare Leadership for their role in implementation.
- Use the Leadership Readiness Self-Assessment in section 2.2 to gather initial information about how well-positioned your managers and supervisors are to support ChYMH Suite implementation. Develop a plan to address any areas that require improvement.
- Clarify overall goals and messaging to ensure that managers and supervisors are ‘on board’, well-informed, and aligned.
- Have a facilitated discussion with the leadership team about their role in implementation. Use the information in section 2.2: “Leadership and ChYMH Suite Implementation” to support this discussion.
- Create a clear plan by completing the Leadership Activities Planning Worksheet (template in Appendix E.)
Commit to clear and ongoing communication to stakeholders.
- Have a facilitated discussion about communication with the Implementation Team. Use CPRI’s practice wisdom in section 2.4: “Communication Planning” to support this discussion.
- Establish a consistent “voice” for communications, based on audience.
- Create a ChYMH Suite Implementation Communication Plan using the information in section 2.4: “Communication Planning” and the template in Appendix G.
Assess training needs and options to create a training plan and team.
- Review mapping and planned use of tools in clinical practice to support training planning.
- Select a training coordinator.
- Follow the steps in section 2.5: “Training Planning” and use the worksheet in Appendix H to create a training plan for initial Assessor and Literacy Training, and for ongoing Assessor, Literacy and Booster training.
- Create a training team.
Launch initial assessor and literacy training to prepare your organization to “Go Live!” with the ChYMH suite.
- Recognize the importance of initial training and how it sets the tone for how staff will feel toward the initiative.
- Have trainers and training coordinators follow the pre-training, “day of”, and post-training steps in section 2.5: “Training Planning” to set themselves up for successful initial training sessions.
Make a plan for how implementation will be monitored and evaluated.
- Commit to ongoing evaluation of implementation by setting targets for sharing reports with stakeholders.
- Decide on measures to evaluate that align with earlier goals and vision. Choose indicators that can tell the story of your journey.
- Create an implementation logic model that will inform the development of an evaluation and monitoring plan.
- Use the Evaluation And Monitoring Plan Template in Appendix K to develop a plan for monitoring implementation process indicators and evaluating outcomes.
- Use the Data Management Plan Template in Appendix L to develop a plan for how data for the Evaluation and Monitoring Plan will be collected and stored.
Footnotes
- footnote[5] Back to paragraph If you like, you can head to Appendix D for a worksheet with space to jot down your notes.
- footnote[6] Back to paragraph To access the Leadership Activities Planning worksheet, head to Appendix E.
- footnote[7] Back to paragraph To access the Risk Management Planning worksheet, see Appendix F.
- footnote[8] Back to paragraph To access the resources mentioned on this page, head to Appendices J, K, and L.