Progress on Ontario’s Provincial Framework for Palliative Care
Read about the progress made towards Ontario’s Provincial Framework for Palliative Care and opportunities for continued improvement.
Ministry of Health
June 4, 2025
Message from the Deputy Premier and Minister of Health
Ontario has established a vision for palliative care that enables individuals with a serious illness, as well as families and caregivers, to receive the holistic, proactive, timely and continuous care they need, to live as they choose and optimize their quality of life. This vision has been articulated through the passing of the Compassionate Care Act, 2020, and the subsequent Provincial Framework for Palliative Care (2021). Since the release of the Provincial Framework, and through the collective efforts of many, substantive progress toward the Provincial Framework’s goals has been achieved.
To demonstrate a continued commitment to improving access to palliative care, the Ontario government has made significant investments, many of which are outlined in this report. This includes committing to the development of more hospice residence beds across the province and additional operational supports to sustain and expand the valuable services these organizations provide. Expanding access to end-of-life care for communities across the province is another step our government is taking to deliver compassionate and specialized care for individuals and their loved ones.
We also know that other investments — such as those in home and community care — support palliative and end-of-life services for individuals who can stay in their homes by maintaining continuity of care, quality of life, and providing adequate support for dying at home or in the community when possible.
I am pleased to report that the number of Ontarians accessing palliative care services has grown by 7.5% from 2021–22 to 2023–24. Additionally, Ontarians are not only receiving care but are accessing it sooner. On average, individuals are now accessing palliative care one month earlier in their illness journey.
While much has been accomplished, more remains to be done. Building on what has been achieved, continued improvements will include spreading and scaling impactful practices across community organizations, continuing to fill data gaps including capturing caregiver experiences, and supporting culturally competent care and inclusion for First Nations, Inuit, Métis and urban Indigenous people, Francophones and persons who are unhoused or vulnerably housed, among others.
On behalf of all Ontarians, I extend my gratitude to all those who continue to advocate for and deliver the person-centered, holistic, proactive, timely, and high-quality palliative care that supports quality of life, through to the end of life.
The Honourable Sylvia Jones
Deputy Premier and Minister of Health
Part I — Introduction
Background
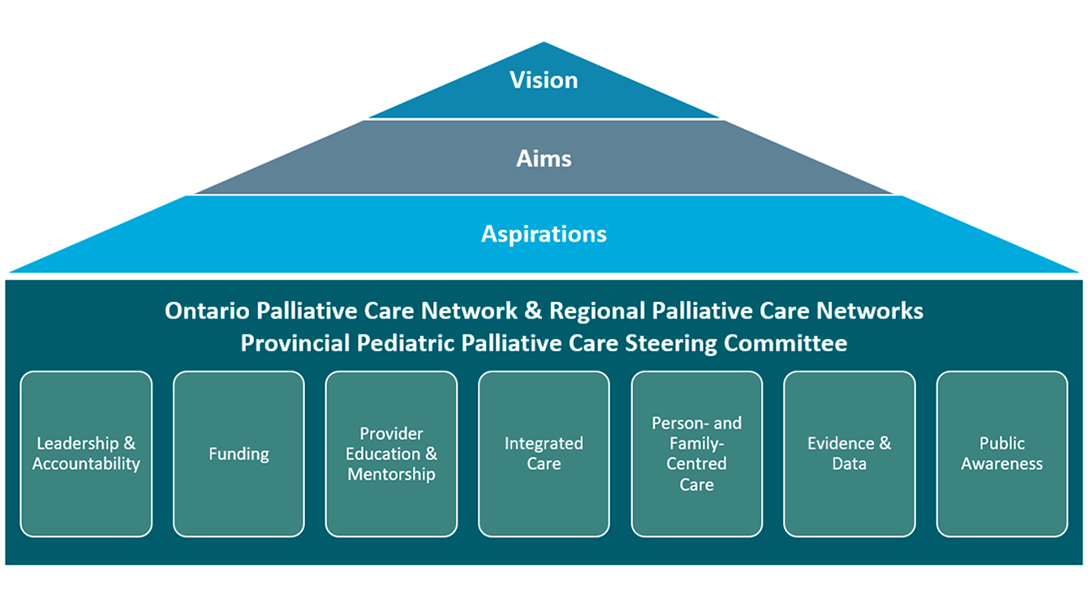
The Compassionate Care Act, 2020 called for the development of Ontario’s Provincial Framework for Palliative Care (the “Provincial Framework”) to support improved access to palliative care for all Ontarians. Developed through extensive stakeholder consultation and released in 2021, the Provincial Framework (visually depicted below) is used to improve how palliative care is planned, delivered, and evaluated in Ontario. The Compassionate Care Act, 2020, also requires the Minister of Health to prepare a report on the status of palliative care in the province within three years after the Provincial Framework’s release (December 2024).
The central vision of the Provincial Framework is as follows:
Adults and children with a serious illness, as well as their families and caregivers, will receive the holistic, proactive, timely and continuous care and support they need, through the entire spectrum of care both preceding and following death, to help them live as they choose and optimize their quality of life, comfort, dignity, and security.
This report summarizes Ontario’s progress toward the Provincial Framework’s vision for success since its release in 2021, and opportunities for continued improvement.
What is palliative care and why does it matter
Palliative care aims to relieve suffering and improve the quality of living and dying for every person with a serious illness. It helps individuals, families and caregivers to:
- address physical, psychological, social, spiritual and practical issues, and their associated expectations, needs, hopes and fears
- prepare for and manage end-of-life choices and the dying process
- cope with loss and grief
- treat all active issues and prevent new issues from occurring
- promote opportunities for meaningful and valuable experiences, and personal and spiritual growth
footnote i
In Ontario, palliative and end-of-life care is integrated into a variety of settings and provided by a range of professionals working together across the health care system.
Access to high quality palliative care benefits individuals, families and caregivers by focusing on quality of life and establishing goals of care centered around what is important to them. Broader access to palliative care also benefits the health care system by ensuring care is managed in the most appropriate setting. For example, when palliative care is delivered in a community setting (for example, patients’ homes, long-term care homes) the likelihood of dying in hospital decreases
Palliative care is often organized at the local level and driven by grassroots initiatives and local networks of providers. This has led to groups of palliative care programs that respond to local needs by building on existing resources rather than meeting a standardized model. Implementation of the Provincial Framework aims to establish an equitable approach to care delivery and assist all Ontarians with accessing palliative care services regardless of where they live.
Performance measurement
Despite the known benefits resulting from a palliative approach to care, there are still gaps in access to services. For example, the Canadian Institute for Health Information’s (CIHI) most recent report on access to palliative care in Canada
Ontario Health monitors and reports on system level indicators that are used to track the influence of palliative care at the provincial, regional and sub-regional level. These indicators can demonstrate how effectively palliative-specific services are being integrated and highlight where attention is required to advance effective practices and service access.
As of 2024, Ontario has seen the following results on three key system use indicators:
- 32% of community dwelling individuals received palliative-specific home care visits in their last 90 days
- 52.6% of decedents had unplanned emergency department visits in their last 30 days
- 50.5% of decedents spent their final days hospital
Since the release of the Provincial Framework, significant investments have helped expand access to palliative care services and strengthen service delivery. As a result, the number of Ontarians accessing palliative care services across all sectors has grown from 75,230 in 2021–22 to 80,912 in 2023–24, representing a 7.5% increase.
In 2023–24, the home care sector increased service volumes by 10%, delivering approximately 2.5 million hours of personal support services and 890,000 nursing visits
The stability in the above three system indicators demonstrates sustained performance under pressure as the system responds to increased demand. It reflects a system that is growing through provincial investments and continues to deliver care while building for the future. As the framework continues to mature, the impact of recent strategic investments is expected to grow. The addition of 96 new hospice beds announced in March 2024, alongside a $44 million investment over three years in Health Human Resource capacity, such as clinical coaches and frontline training, have not been fully reflected in these indicators as they are still in early stages of implementation.
In continuing to act on the government’s commitment to provide better palliative care, Ontario, in collaboration with system partners, is making concrete steps to improve access, equity, and the quality of palliative care services for Ontarians. The chart below provides a snapshot of key investments and activities, and Part II of the report provides further details. Additionally, regional achievements have been highlighted in Appendix A.
Highlights of Ontario’s progress to increase access to palliative care since 2021
| Leadership & accountability |
|
|---|---|
| Funding |
|
| Provider education & mentorship |
|
| Integrated care |
|
| Person-centred care |
|
| Evidence & data |
|
| Public awareness |
|
Part II — Progress report
System level progress
Ontario continues to make strides to increase access to health care resources for all Ontarians where and when they need them. Enhancing access to a palliative approach to care can be strengthened at the system level through appropriate integration of health care services and decreasing silos.
Change is needed across multiple sectors to support an integrated approach to care. The following are examples of actions taken by the Ontario government since 2021 that will improve the likelihood of accessing and maintaining palliative care in any setting:
- Expanding access to key services to provide people of all ages with the right care, in the right place through Your Health: A Plan for Connected and Convenient Care.
- Establishing Ontario Health Teams (OHTs) as groups of providers that coordinate and deliver care for their local community. OHTs are focused first on connecting patients to primary care, supporting seamless home and community care, and improving outcomes for people with chronic illnesses.
- Investing in home care services to get more people connected to care in the comfort of their own home and community.
- In the 2022 Budget, the government announced a plan to invest $1 billion over three years to support the expansion of home and community care services and workforce compensation.
- In 2023, the government accelerated investments in home care, as part of the 2023 Budget, bringing funding up to $569 million, including nearly $300 million to stabilize the home and community care workforce.
- In the 2024 Budget, the government invested an additional $2 billion over three years to boost the accelerated $1 billion committed in 2023, support earlier investments in the home and community care workforce, and stabilize expanded services.
- Taking the next step to better connect and coordinate people’s care with the establishment of Ontario Health atHome.
- On June 28, 2024, the Convenient Care at Home Act, 2023 was proclaimed into force, amalgamating the 14 Local Health Integration Networks (LHINs), operating as Home and Community Care Support Services organizations into a single organization - Ontario Health atHome.
- Ontario Health atHome will continue to support the delivery and coordination of home and community care services and long-term care placement across the province. This will make it easier for people to connect to the services they need, including home and community care services, long-term care and other placement management services, and information and referrals to other health and social services.
- Investing in community care services which play an important role in helping people live safely and independently. These services include personal support services, homemaking services, and community support services (CSS) including meals, transportation, caregiver support and respite services.
- In 2022–23, Ontario invested nearly $100 million over three years to expand community care. This base investment of $33.25 million starting in 2022–23 will stabilize and enhance sustainability for community services.
- In 2023–24, approximately $100 million in new funding was provided to the community care services sector and to expand assisted living services.
- Introducing a new legislative framework to govern long-term care services. On April 11, 2022, the Fixing Long-Term Care Act, 2021 (FLTCA) and its supporting regulation came into force. The FLTCA outlines expanded palliative care requirements to align with a broader, more holistic approach to palliative care that is not solely focused on end-of-life care.
Progress on implementation of the Provincial Framework
In addition to the system-level progress highlighted above, Ontario continues work on implementation of the Provincial Framework to support the delivery of high-quality palliative care services in communities. The Provincial Framework can be utilized for palliative care service delivery, to guide future policy and program design, and to assist in funding decisions to improve palliative care for all individuals who would benefit.
Building on considerable work by health care partners over many years, the Provincial Framework outlines seven building blocks, with related goals and initial actions to move toward Ontario’s vision for access to palliative care. The progress toward the Provincial Framework’s vision for success is the result of the collective impact of many provincial, regional, and local partner organizations.
1. Leadership & accountability
As described in the Provincial Framework:
Effective and efficient palliative care service design and delivery requires strong and visible leadership. Accountability models and structures can drive consistent access and delivery of palliative care across the province and ensure value for money. Key accountability mechanisms include performance metrics, policies, guidelines, standards, and funding.
OPCN has a provincial oversight structure (see below) and acts as the province’s principal advisor on palliative care. OPCN is supported by the Provincial Palliative Care Program, six Ontario Health Regions, and sub-regional palliative care networks.
OPCN oversight structure
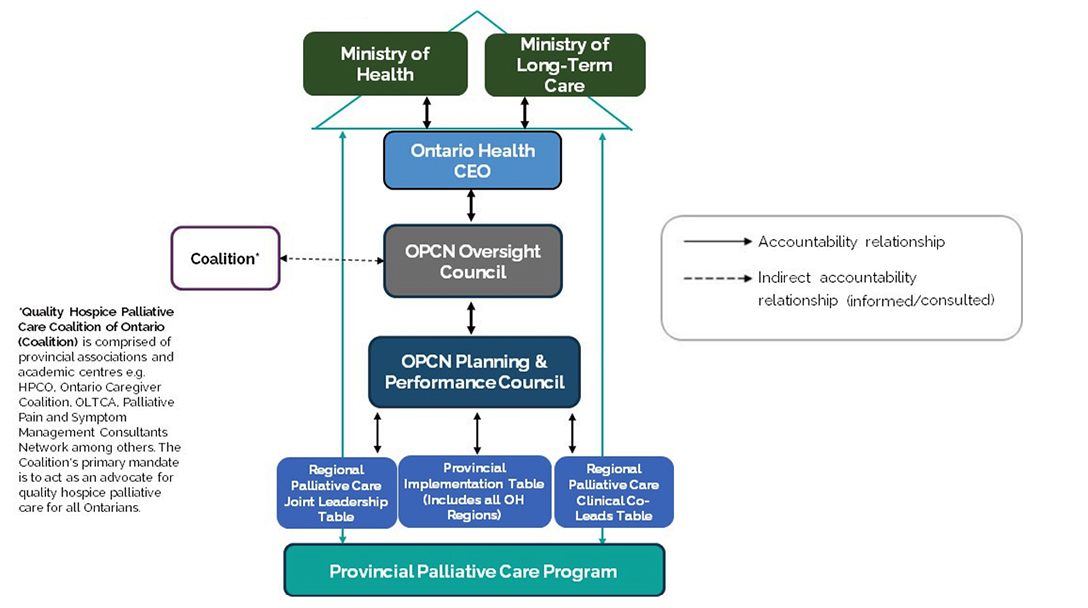
OPCN, supported by the Provincial Palliative Care Program, has developed a strategic policy document, the Palliative Care Health Services Delivery Framework (Delivery Framework). Developed through broad consultation and identifying best practices, the Delivery Framework provides actionable recommendations to improve care integration. The Delivery Framework is implemented through the structure depicted in the diagram above. Furthermore, Ontario Health supports in improving access to palliative care.
Ontario Health’s role is to connect, coordinate and modernize the health care system, including the shift to OHTs to organize and deliver care that is more connected to individuals in their communities. In this context, the Provincial Palliative Care Program and the Ontario Health regions are accountable for collaborative planning and the considerable work underway to build system capacity, encourage integration and support local teams to deliver seamless palliative care.
Future work will use the established leadership and accountability structures to continue work with Ontario Health Teams, align with home care modernization, and support individual health care organizations, including long-term care homes, to implement the policy direction from the Provincial and Delivery Frameworks.
2. Funding
As described in the Provincial Framework:
Funding is essential for equitable, accessible and sustainable palliative care supports and services for Ontarians. Funding allocations should consider support for health human resource capacity needs, access to equipment and supplies across care settings, as well as to psychosocial, spiritual, mental health, grief and bereavement services, education and mentorship. The pillar goals include completing a comprehensive analysis of current funding across all settings, creating a model of resources needed for integrated care, and developing strategies to ensure funding is equitably allocated across settings and populations.
To support implementation of the Delivery Framework, a funding and accountability analysis and system planning work is currently underway for the province. Beginning with grief and bereavement services, system planning activities will assess current and future community needs for palliative care and identify gaps in access to resources.
Since 2021, Ontario has made significant investments with an aim to improve equitable access to palliative care in the community. Some examples include:
- Adding more hospice residence beds to increase end-of-life care options for individuals across the province.
- Through Budget 2024, Building a Better Ontario, the Ontario government has committed to adding up to 84 new adult beds and 12 pediatric beds, bringing the total to 768 planned beds to meet current and future capacity needs. This investment includes allocations for operational and capital funding. Allocation of the new beds will be determined using established evaluation criteria which consider factors such as local demand, current state capacity, equity, and organizational readiness.
- In 2023, adding 23 new hospice beds through Ontario’s Plan to Stay Open: Health System Stability and Recovery to address the immediate pressures facing the health system and support care for end-of-life patients outside of hospitals.
- Additional operational funding to sustain the hospice residence sector for the future and address the increasing pressures facing the health system.
- In June 2023, Ontario committed an additional $53.8 million to increase operational funding support by 45% for all approved hospice beds in the province, plus an additional increase for hospice beds in small facilities for the 2023–24 and 2024–25 fiscal years.
- New funding to stabilize and expand community-based grief and bereavement services across the province. To date, funding has been allocated to more than 120 organizations.
- Early access to support for the bereaved assists in preventing more complex grief reactions and the need for clinical interventions later in the bereavement process.
The government’s additional investments in care in the community, including home care and hospice residences, will increase Ontarians’ access to high quality palliative care in their setting of choice, making it possible for more people to die at home or in home-like environments such as hospices, rather than in hospital.
In order to continue advancing the funding pillar goals, ongoing efforts will focus on assessing existing palliative care funding models, including identifying where further investments are needed. Next steps in system planning will focus on a provincial model for pediatric palliative care and on allocation of the newly committed hospice residence beds.
3. Provider education and mentorship
As described in the Provincial Framework:
Service providers across care settings benefit from the necessary knowledge and skills to deliver high-quality palliative care when and where it is needed. Education and mentorship opportunities build palliative care capacity, and ensure providers have the competency to identify those who would benefit from a palliative care approach.
Organizations and individual health care providers across Ontario are actively engaged in education to improve palliative care knowledge and skills.
Leveraging Ontario’s Palliative Care Competency Framework (2019), examples of key accomplishments that have increased access to palliative care education since the release of the Provincial Framework include (but are not limited to):
- In early 2022, to address the training needs of home care providers, the Provincial Palliative Care Program partnered with Home Care Ontario, Home and Community Care Support Services (now Ontario Health atHome) and Pallium Canada to fund and make available online training modules for over 400 nurses and personal support workers.
- Since 2021–22, the Provincial Palliative Care Program worked with Regional Clinical Co-Leads to develop tools and resources to support the integration of palliative care for the Ontario Health Teams.
- Provincial funding in 2023–24, that supported primary level palliative care education for over 9,600 providers in at least 100 hospitals, 53 LTC homes, 45 community organizations, 26 hospices, all Regional Cancer Programs and Regional Pediatric Academic Health Sciences Centres.
- In the North East, an innovative partnership has been developed with the Northern Ontario Medical School to support physician training and education on palliative care.
- The Provincial Palliative Care program funded the Center for Education and Research on Aging and Health (CERAH) to implement culturally relevant palliative care education for 80 health and social care providers caring for First Nations, Métis, Inuit, and urban Indigenous people. Open access education will also be provided in 2025. These resources focus on educating healthcare providers in the community and long-term care sectors, including interdisciplinary providers who serve these communities.
The impact of education, including helping service providers understand the benefits of palliative care and how to identify palliative care needs earlier, is beginning to emerge. Since 2021, on average, Ontarians are accessing palliative care one month earlier in their illness journey.
4. Integrated care
As described in the Provincial Framework:
To address an individual’s full range of needs, palliative care should be introduced early and integrated with chronic disease management throughout the illness trajectory. Aligning with the goals of integrated care delivery through Ontario Health Teams, 24/7 palliative care requires barrier-free communication and coordination between members of the interdisciplinary care team and across settings to improve access, ensure smooth transitions and facilitate continuity of care.
As envisioned in the Provincial Framework, the Delivery Framework will consist of three models:
- Pediatric palliative care across all settings
- Care for adults in the community, including long-term care
- Care for adults in hospital
Development and implementation considerations for each of the models will occur on a consecutive basis, beginning with adults in the community. Work in models for pediatrics and adults in hospital are in development with adults living in the community implementation underway.
Implementation of the model of care for adults living in the community is underway, and intends to:
- Build the palliative care knowledge and skills of health care providers in community organizations by optimizing the use of health human resources;
- Deliver seamless palliative care to patients and residents through integration, role clarity and better connections between providers to support broader integration and coordination and;
- Provide patients, residents and their families/caregivers with timely, equitable access to high-quality care as close to home as possible.
Since the launch of the community model of care, 34 organizations have received funding to hire clinical coaches who will work with community providers to support projects aligned to the model of care.
The model of care for adults in the community includes recommendations to support culturally competent care and inclusion for First Nations, Inuit, Métis and urban Indigenous people, Francophones and persons who are unhoused or vulnerably housed. Some examples of initiatives to address their specific needs include but are not limited to:
- A 2024–25 call for expressions of interest launched to allocate funding to 26 organizations meeting the needs of First Nations, Inuit, Metis and urban Indigenous people supporting self-determined approaches to address palliative care needs.
- In April 2024, eight new hospice residence beds serving the Franco-Ontarian community were opened in Ottawa.
- Nine communities across Ontario are currently working to improve access to palliative care for those with unstable housing by participating in a national improvement collaborative led by Healthcare Excellence Canada and the Canadian Partnership Against Cancer to improve equity in access to palliative care.
Leading projects
Within the Leading Projects initiatives aimed at implementing and testing models of home and community care delivery, there are two that have a particular focus on integrated care for palliative care populations within their Ontario Health Teams. These initiatives aim to ensure early identification of palliative care patients and enhancement of palliative care competencies. These models are testing a team-based approach to care that enables timely connections and consultations among care providers with different expertise, including in palliative care, in order to ensure a patient’s needs are addressed in a coordinated manner.
Patient Care Models for 9-1-1 palliative care patients
Through Your Health: A Plan For Connected and Convenient Care, Ontario is expanding patient care models (PCMs) that offer paramedics more flexibility to provide eligible patients who call 9-1-1 with the most appropriate care in the community, rather than in emergency rooms.
Since 2020, 9-1-1 PCMs have allowed paramedics to treat and refer or transport palliative patients to an alternate destination. Participation in the PCM initiative is voluntary for paramedic services.
- The Treat and Refer model provides eligible palliative patients calling 9-1-1 with the option to be treated by paramedics on-scene for symptom management and then receive follow up care from their palliative team or be referred by paramedics to an appropriate care provider for follow-up care.
- The Alternate Destination model provides eligible palliative patients calling 9-1-1 with the option to be treated by paramedics on-scene as needed, and then to be transported by paramedics to a local hospice for care.
Community Paramedicine
The Ministry of Long-Term Care currently funds the Community Paramedicine for Long- Term Care (CPLTC) program, which supports vulnerable seniors and individuals in the community who are on a waitlist for LTC. The program leverages specially trained community paramedics to provide assessments, diagnostic testing, and treatments, including palliative care, to seniors across the province in the safety and comfort of their own homes. CPLTC has been shown to reduce avoidable emergency department visits and hospital admissions that can adversely impact palliative care patients.
The Ministry of Health also provides funding for Community Paramedicine, separate from LTC, that includes home visits to support individuals receiving a palliative approach to care.
Having achieved the initial goals related to the model of care for adults in the community, the next steps for this building block include:
- Expanding the number of community organizations, such as primary care providers, long-term care homes, and community support service providers.
- Implementing the model of care recommendations with the aim of increasing care in the community and reducing reliance on acute care services.
- Evaluating the reach and impact of the model for adults in the community.
- Planning the dissemination of the model for adults in hospital settings, and the model for children across all settings.
Concurrently, opportunities to improve partnerships and linkages, and support other Ontario Health initiatives such as home care modernization and OHTs, will continue.
5. Person and family centered care
As described in the Provincial Framework:
High quality palliative care includes patients, residents and families/caregivers as active participants in decisions, is available 24/7, is provided by an interdisciplinary team and addresses the full range of an individual’s needs in a culturally appropriate manner. The Provincial Framework called for identification of gaps and the best practices to address them to be implemented, scaled and spread.
Implementing the recommendations in the Delivery Framework is central to advancing person and family-centered care. Examples of initiatives underway to address gaps include but are not limited to:
- In 2024–25, the province supported the Ontario Centres for Learning, Research and Innovation’s (CLRI) Communication at End-of-Life Training Fund (CEoL Fund). The Collaborative Project to Sustain a Palliative Approach to Care in Long-Term Care under the CEoL Fund is driving meaningful change in Ontario’s long-term care homes by integrating a palliative approach to care, with a strong emphasis on person and family centered care. The project will enhance personalized care plans that respect residents' unique needs and cultural backgrounds while actively involving families. Continuous feedback loops will enable LTC homes to adapt practices to the evolving needs of residents and their families.
- More than 120 organizations have received new funds through the Ministry of Health to support increased grief and bereavement service capacity. Recognition of loss and grief through the provision of bereavement support is a core component of the palliative continuum of care.
- The Systemic Treatment Program at Ontario Health (Cancer Care Ontario) undertook a multi-year strategy to increase the use of Goals of Care conversations. Interventions included a provincial quality metric, a Goals of Care Toolkit for Oncology Settings, and a two-year centrally led, locally implemented quality improvement project. Early results suggest that these interventions are leading to a significant decrease in the use of systemic treatment at the end of life, which is an established success metric for quality of care.
- In its 2019–23 plan, the Ontario Renal Network (ORN) outlined a strategic objective to strengthen the early identification of and support for people who would benefit from a palliative approach to care. By using a Comfort- Focused Kidney Care (CKC) approach to maximize comfort and quality of life while minimizing adverse events for patients, there has been an increase in the proportion of patients with end-stage kidney disease receiving CKC from 6% to 11%. The ORN’s Ontario Renal Plan 4 (2024–28) will build on this success with a commitment to improve the delivery of comfort-focused kidney care in partnership with primary care, nephrology care and palliative care teams. ORN will continue to share data with Regional Renal Programs to support their quality improvement initiatives.
Health care partners across sectors continue to collaborate to develop provincial, regional and local solutions to gaps in care. The impact of these collective efforts is beginning to emerge — since 2021, the number of Ontarians accessing palliative care services has increased from 75,230 in 2021–22 to 80,912 in 2023–24, representing a 7.5% increase in patients and their families with access to palliative care services.
6. Evidence and data
As described in the Provincial Framework:
High-quality palliative care requires data systems to support ongoing system planning, quality improvement, research, evaluation and decision-making. Organizations can participate in shared learnings to facilitate equitable access for diverse and underserved populations. Data and research should respect Indigenous data governance principles such as the First Nations Principles of OCAP® (ownership, control, access, and possession).
Since 2021, significant progress has been made on data collection and performance measurement.
The Provincial Palliative Care Program:
- Created a Palliative Care Measurement Strategy in 2023–24 which identifies current gaps and advocates for integration of data systems to drive continuous improvement, and advance high-quality palliative care.
- Developed and implemented a measurement approach specifically for the Adult Community Model of Care implementation that includes new data collection tools and captures the patient and family voice.
- Distributed a quarterly performance summary report and an annual regional profile report that support local and regional improvement initiatives.
Ontario is also participating in Pallium Canada’s Canadian Palliative Care Atlas research project by providing a comprehensive view of palliative care supports, services and assets across the province. Atlases are widely used tools to describe current state, highlight excellence and outline gaps and opportunities. Ontario’s participation will provide additional information on where palliative resources are available across the province to inform future planning.
To better capture the experience of accessing grief and bereavement services and to support system planning, Hospice Palliative Care Ontario has been funded to develop a set of provincial indicators for these important services.
While significant progress has been made on coordinating, standardizing and using data for system improvement, more can be done. Future work aims to fill data gaps such as the individual and caregiver reported experience through implementation of Caregiver Voices, define and implement new provincial indicators and continue to use best available data — such as asset maps and utilization information — for system planning.
7. Public awareness
As described in the Provincial Framework:
Improving the public’s general understanding of palliative care, the role of services, and available supports for individuals and their families and caregivers is important for reducing stigma, normalizing death and dying, as well as empowering individuals to access palliative care services, and manage their care
Advance care planning (ACP) workshops and resources continue to be available for Ontarians through a range of organizations such as Speak Up Ontario, Hospice Palliative Care Ontario, and the Ontario Caregiver Organization.
As part of its work to improve access to palliative care the CLRI is delivering a Palliative Care Series for Families and Carers to raise public awareness about palliative care approaches in long-term care. The program also provides Peer Support in collaboration with Family Council Ontario (FCO) and access to a comprehensive resource library. As a result of the sessions, 81% of participants reported increased knowledge and a better understanding of the benefits of palliative care.
Taking active roles in caring for others and raising awareness of end-of-life issues, Compassionate Communities are groups of citizens who feel empowered to engage with and increase understanding about the experiences of those living with a serious illness, caregiving, dying and grieving. Compassionate Communities are another way that public awareness of palliative care and access to support at the end of life is being improved. A growing grass roots movement across Canada, there are currently more than 40 Compassionate Communities active in Ontario.
Future efforts will continue to promote ACP, to help Ontarians access resources to support their planning for future care, and to increase awareness of palliative care and normalize conversations around death. There are also opportunities to explore how emerging public-health approaches to palliative care such as Compassionate Communities can be encouraged and supported.
Conclusion
Sustained collective efforts have resulted in more Ontarians accessing palliative care. There is work going on at all levels and in all sectors of the health care system to continue to close gaps in access and quality. This momentum will continue to be leveraged to support additional improvements.
Using the Provincial Framework as a guide, efforts will continue to spread and scale impactful practices in the community, improving integrated, person and family-centered care. This includes continuing to improve access to culturally competent care and inclusion for First Nations, Inuit, Métis and urban Indigenous people, Francophones and persons who are unhoused or vulnerably housed through spreading and scaling best- practices; educating health service providers on culturally competent care; and engaging with Indigenous communities to develop a culturally appropriate model of care for children and support for self-determined palliative care initiatives. Efforts will also continue to fill data gaps, such as patient and family experience measures, to inform system planning and improvement.
Appendix A: Summarized regional initiatives
- Ontario Health East Accomplishments
- Ontario Health Central Accomplishments
- Ontario Health North East Accomplishments
- Ontario Health North West Accomplishments
- Ontario Health Toronto Accomplishments
- Ontario Health West Accomplishments
| Framework building block | Ontario Health East Accomplishments |
|---|---|
| Leadership and accountability |
|
| Funding |
|
| Provider education and mentorship |
|
| Integrated care |
|
| Person and family centered care |
|
| Evidence and data |
|
| Public awareness |
|
| Framework building block | Ontario Health Central Accomplishments |
|---|---|
| Leadership and accountability |
|
| Funding |
|
| Provider education and mentorship |
|
| Integrated care |
|
| Person and family centered care |
|
| Evidence and data |
|
| Framework Building Block | Ontario Health North East Accomplishments |
|---|---|
| Leadership and Accountability |
|
| Funding |
|
| Provider Education and Mentorship |
|
| Integrated Care |
|
| Person and Family Centered Care |
|
| Evidence and Data |
|
| Public Awareness |
|
| Framework building block | Ontario Health North West Accomplishments |
|---|---|
| Leadership and accountability |
|
| Funding |
|
| Provider education and mentorship |
|
| Integrated care |
|
| Person and family centered care |
|
| Evidence and data |
|
| Public awareness |
|
| Framework building block | Ontario Health Toronto Accomplishments |
|---|---|
| Leadership and accountability |
|
| Funding | Distributed funding:
|
| Provider education and mentorship |
|
| Integrated care |
|
| Person and family centered care |
|
| Evidence and data |
|
| Framework building block | Ontario Health West Accomplishments |
|---|---|
| Leadership and accountability |
|
| Funding |
|
| Provider education and mentorship |
|
| Integrated care |
|
| Person and family centered care |
|
| Evidence and data |
|
| Public awareness |
|
Footnotes
-
footnote[i]
Back to paragraph
Advancing High Quality, High Value Palliative Care in Ontario: A Declaration of Partnership and Commitment to Action [Internet]. Queen’s Printer of Ontario; 2013.
Accessed at: https://hpco.ca/qhpcco/Declaration_of_Partnership_English.pdf - footnote[ii] Back to paragraph Tanuseputro P, Beach S, Chalifoux M, Wodchis WP, Hsu AT, et al. (2018) Associations between physician home visits for the dying and place of death: A population-based retrospective cohort study. PLOS ONE 13(2): e0191322. https://doi.org/10.1371/journal.pone.0191322
- footnote[iii] Back to paragraph Sutradhar R, Barbera L, Seow H-Y. Palliative homecare is associated with reduced high- and low-acuity emergency department visits at the end of life: A population-based cohort study of cancer decedents. Palliative Medicine. 2017;31(5):448-455. doi:10.1177/0269216316663508
-
footnote[iv]
Back to paragraph
Canadian Institute for Health Information. Access to Palliative Care in Canada, 2023.
Ottawa, ON: CIHI; 2023 - footnote[v] Back to paragraph Kimberley Widger, Dawn Davies, Adam Rapoport, et. al. (2016). Pediatric palliative care in Canada in 2012: A cross-sectional descriptive study. CMAJ Open, 4 (4) E562-E568; DOI: 10.9778/cmajo.20160054
- footnote[vii] Back to paragraph Ontario Health, Quality Measurement and Evaluation, (April 2025), Number of Ontario patients who accessed palliative care. Internal Report, Unpublished.
- footnote[viii] Back to paragraph Ontario Health, Quality Measurement and Evaluation, (April 2025), Days From First Palliative Care Contact to Death. Internal Report, Unpublished.
- footnote[ix] Back to paragraph Ontario Health, Quality Measurement and Evaluation, (March 2025), 2024–25 Performance Summary Report Q2, Internal Report, Unpublished.