Promoting Partnerships Between Mental Health and Education to Improve Outcomes
Abstract
Stigma and marginalization is a significant issue related to children’s mental health and directly impacts educational success. Specialized information sessions for educators and in-service presentations for peers were conducted in an attempt to improve social acceptance and understanding of children with Tourette Syndrome and Associated Disorders (TS+).
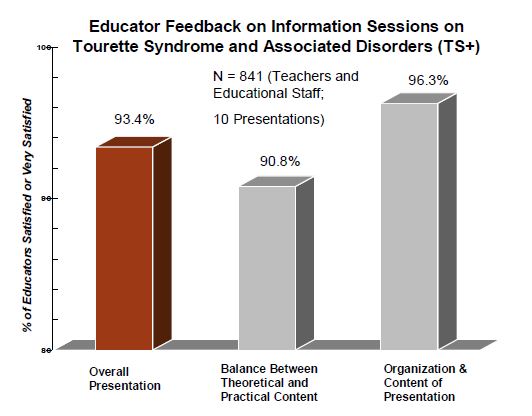
Feedback from 841 teachers indicated very high satisfaction rates with the educator information sessions. Post peer in-service data from clients indicated increased peer acceptance, and teachers reported a slight reduction in negative peer reactions to clients’ tic behaviours. Additionally, teacher reports indicated significant reduction in client internalizing behaviour following treatment groups for the children with TS+.
Purpose
The prevalence of diagnosed Tourette Syndrome (TS) in the general population is estimated to be 1%. However, as symptoms peak in adolescence, estimates are much higher and range from 3.8% in mainstream classrooms and 7% in special education (Kurlan et al., 2001). TS shows high co-morbidity with other disorders, such as Attention Deficit-Hyperactivity Disorder, Obsessive-Compulsive Disorder, other anxiety and Mood Disorders, Depression, and Conduct and Antisocial Disorders. The resulting adjustment problems, as well as developmental and learning disorders can be debilitating for youth. As such, there is a significant need for resources and treatment for those affected by TS+.
A key goal of the Ministry of Children and Youth Services (MCYS) is that “Every young person graduates from secondary school”. To make this a reality, MCYS emphasizes the necessity of fostering strong partnerships with the education sector to improve outcomes for youth. The Brake Shop, a specialized outpatient clinic at CPRI, a tertiary mental health treatment centre, has successfully fostered a strong relationship between mental health and the education sector to improve peer acceptance and educational outcomes for youth with TS+.
Theoretical framework
The marginalization of youth with TS+ by their peers is an area of immense concern. The anxiety and embarrassment experienced by youth with TS+ due to a lack of peer understanding can lead to extreme social withdrawal. Studies of self-report of victimization for youth with TS+ (e.g., Packer, 2005) tend to mirror peer reports of negative attitudes toward fellow students with tics. As a result, the majority of children with TS+ tend to avoid participating in social activities (Debes et al., 2010). Social rejection in school is a problem with far-reaching consequences such as low academic achievement, truancy and dropping out of school. The extant literature overwhelmingly supports the need for additional educational resources for children with TS+ as well as for their teachers and peers.
The present study sought to alleviate negative attitudes toward youth with TS+ through education and disclosure. Past research (e.g., Woods & Marcks, 2005; Maracks et al., 2007; Holtz & Tessman, 2007) has investigated the effects of peer education on acceptance and understanding of TS with promising results. The current study presents results from an evaluation of educational sessions, in which the key outcome is a change in peer acceptance, reduction of bullying, victimization, and marginalization of youth with TS+ as reported by teachers and children.
Method
Procedure
Specialized information sessions were conducted with educators, and in-service presentations were offered to peers and teachers, in conjunction with the identified child and their family. The purpose of the information sessions for teachers was to increase professional competence in working with children with TS+.
The peer in-service sessions were offered to children at the school of the identified child, to increase knowledge, peer acceptance, and reduction of social stigma towards the youth with TS+. For young children (e.g., < 8 years), the in-service was often conducted at an individual classroom level, while for older children (e.g., > 9 years), the presentation occurred in a larger format (e.g., school assembly). The in-service included psychoeducation about a range of symptoms, such as tics, inattention, impulsivity, obsessions and compulsions, sensory processing dysfunctions, and behaviour “rages”. Attendees included students, teachers, educational support staff, and the identified child with their family.
Measures
Parent and Teacher Report: Parent data from the Child Behaviour Checklist (CBCL; Achenbach & Rescorla, 2001) and teacher data from the Teacher Report Form (TRF; Achenbach, 1991) was collected for all children prior to, and after, their involvement with the Brake Shop specialized clinic for children with TS+.
Educator information session
Participating staff completed a form soliciting feedback on the information session on TS+ addressing: balance between theoretical and practical information, perception of the content and organization, and overall satisfaction.
Peer in-service
Client Ratings of Peer Disruptions – Post-Measure. At least one- month after the peer in-service, feedback was solicited inquiring whether the presentation made things better at school, with additional items addressing friendships, peer acceptance, and social stress.
Teacher Ratings of Peer Disruptions due to TS+ – Pre & Post. Before and at least one month following the peer in-service teachers were asked to report:
- # of child complaints to teachers about peer treatment;
- # of suspensions due to peer incidents;
- # of times the child was sent to the office due to peer incidents.
Data on peer reactions to tics was also requested pre and post peer in-service, but only 7 teacher reports were returned. The data described here is mainly cross-sectional, collected in parts from 2007-2011. Across all measures data was obtained for a total of 96 Brake Shop clients.
Results
Parent and teacher report
The complex mental health issues of this population were illustrated using parent and teacher reports. Results were all significant when T- scores were compared against a value of 60 (the CBCL cut-off from normal to clinical range of significance).
Paired t-tests indicated that teachers noted a significant decrease in internalizing behaviour, but not in other areas for children participating in Brake Shop treatment programs.
Educator information sessions
Feedback indicated a very high rate of overall satisfaction with the information presented on TS+.
Peer in-service
Post peer in-service data was collected, with the majority reporting an overall increase in peer acceptance and a decrease in marginalization following the in-service.
A challenge was obtaining post in-service teacher data. Prior to the in- service, 39 teachers reported on complaints, client suspensions/office visits due to peer incidents. However, only 16 teachers provided post data. Paired t-tests indicated no difference between pre and post in- service data, but a larger sample may be necessary for differences to emerge. Following the peer in-service, 16 teachers were asked by phone how often the child’s tics result in peer disruptions. A one- sample t-test indicated that teachers rated this significantly low in the “Rarely” range, M= 2.06, SD= .85, t(15) = -4.39, p= .001. Data helped corroborate the clients’ perception of increased peer acceptance following the in-service.
Parent and Teacher
Complexity of Brake Shop Clients at Beginning of Treatment -Comparison to T Score of 60 (Clinical Threshold)
Parent Report Form
- Internalizing Behaviour: M= 67.59; SD= 9.43, p< .001
- Externalizing Behaviour: M= 66.25; SD= 9.98, p< .001
- Total Problems: M= 70.73; SD= 7.18, p< .001
Parent Report Form - Total Problems
- Internalizing; Externalizing; Total Problems: All Significant Results
Teacher Report Form (Pre-Post Treatment)
- Significant Decrease in Internalizing Behaviour: t(15) = 2.65, p< .05
- No Significant Decrease in Externalizing Behavior or Total Problems: t(15) = 2.65, p< .05
Educator feedback
Peer in-service
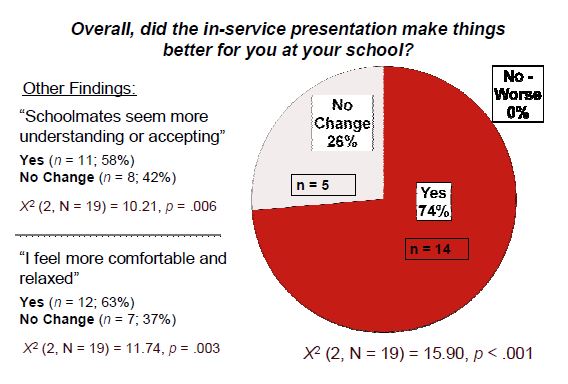
Clinical significance
The suppression of all TS+ symptoms due to teasing/embarrassment (i.e. holding in tics) does far more damage to attention, energy, and self- esteem than simply releasing symptoms. Educational personnel are informed that more tics, rather than less, may surface after the in-service. The rationale is that an increase in symptoms may indicate improved self- comfort (i.e. fewer internalizing problems) rather than exacerbation of the condition. The post in-service client report supports this theory as the youth reported feeling more “relaxed and comfortable” in school. The teacher report of decreased internalizing behaviour is also consistent with this finding, suggesting an increased self-comfort in the social setting.
Past research indicates that peer acceptance of tic behaviour is integral to the well-being of children with TS+. The methods in this presentation to inform peers / educators regarding TS+ were successful in reducing marginalization and stigma. These findings will be useful in extending evidence-based treatment groups and school assembly programs to wider geographical areas, and improving educational outcomes for other youth populations at-risk. Future studies to examine long-term effects of peer education on academic achievement of youth with TS+ may provide further support for the role of social acceptance in school success.
Select references
Debes, N., Hjalgrim, H., & Slov, L. (2010). The presence of Attention-Deficit Hyperactivity Disorder (ADHD) and Obsessive-Compulsive Disorder worsen psychosocial and educational problems in Tourette Syndrome. Journal of Child Neurology, 25, 171-181.
Holtz, K. & Tessman, G. (2007). Evaluation of a peer-focused intervention to increase knowledge and foster positive attitudes toward children with Tourette Syndrome. Journal of Developmental Physical Disabilities, 19, 531-542.
Packer, L. (2005). Tic-related school problems: Impact on functioning, accommodations, and interventions. Behavior Modification, 29, 876-899.
Woods, D. & Marcks, B. (2005). Controlled evaluation of an educational intervention used to modify peer attitudes and behaviour toward persons with Tourette’s Syndrome. Behavior Modification, 29, 900-912.