Guide to developing your COVID-19 workplace safety plan
Learn how you can create a plan to help protect your workers and others from novel coronavirus 2019 (COVID-19).
Overview
This guide will help you use current public health and workplace health and safety information to develop a plan and put controls into place to help make the workplace safer for everyone.
You can use the workplace safety plan builder to help create your COVID-19 workplace safety. All employers are encouraged to review and update their safety plan regularly.
As an employer it’s your responsibility under the Occupational Health and Safety Act to take every precaution reasonable in the circumstances to protect a worker.
Employers are not required to send their plan to the Ministry of Labour, Training and Skills Development and the ministry will not provide comments on safety plans sent in. During an inspection of your workplace, an inspector or compliance officer could ask whether you have developed a safety plan and may ask to see it.
Discuss and share your safety plan with everyone at work, including:
- workers
- unions
- supervisors
- health and safety representatives or members of joint health and safety committees (JHSCs)
- contractors
- suppliers
This guide does not replace the Occupational Health and Safety Act or the Employment Standards Act and their regulations and should not be used as or considered legal advice. Health and safety inspectors and employment standards officers apply the law based on the facts in the workplace.
Develop your COVID-19 safety plan
Key sources of information
It’s important that you talk to workers and your JHSC members or health and safety representatives, if any, for their input on the plan. Share the plan with all workplace parties when it is done. This will help ensure your workers and others understand how you plan to manage the risks of COVID‑19 .
Check the resources to prevent COVID‑19 in the workplace for sector-specific information and examples of controls that apply to your type of workplace. These documents may be helpful as you develop your plan. Visit the webpage regularly to check for the latest information.
Make sure you continue to follow any provincial requirements under the Reopening Ontario (A Flexible Response to COVID‑19 ) Act and any local public health orders. Find out about the latest updates in public health measures, advice and restrictions.
Understand COVID‑19 risks
The first step to control risks in a workplace is to identify them. For COVID‑19 , the risks are related to how the virus spreads.
COVID‑19 primarily spreads from person-to-person through respiratory droplets created by a person who is infected. Respiratory droplets vary in size from large droplets that fall to the ground rapidly near the person, to smaller droplets, sometimes called aerosols. The droplets are created when a person:
- breathes
- talks
- sings
- shouts
- coughs
- sneezes
The virus can also be spread indirectly through contaminated surfaces or objects.
The key risk factors for COVID-19 transmission include:
- close proximity - working close to others
- longer exposure - spending more time with potentially infected people
- crowded places - having more people in a space
- closed spaces - indoor spaces with less fresh air (working indoors is riskier than working outdoors)
- forceful exhalation – activities that cause people to breathe more deeply, such as physically demanding work, speaking loudly and singing
Each additional risk factor in the workplace increases the risk of transmission. Not having any of these factors does not mean there is no risk of transmission.
The risk of severe health outcomes is not the same for all workers. The risk increases with age and is higher for people with certain medical conditions.
It is possible for COVID‑19 to be spread by people who do not have any symptoms, including people who have been vaccinated. Act as if everyone is infected when setting up controls.
Control COVID‑19 risks in the workplace
Control measures are the steps you take to reduce the risks to your workers. With an infectious disease like COVID‑19 your controls can help to break the chain of transmission of the virus and reduce the risk of a workplace outbreak.
Your controls should address the key risk factors for COVID‑19 transmission in your workplace.
The most effective way to stop the spread of COVID‑19 is to limit interactions between people. All workers who can work from home should continue to do so. This is an important way to both protect these workers and help protect those who do have to go into the workplace.
For workers who must be in the workplace, there are a variety of control measures to help reduce the risk of transmission. These measures help to protect workers in different ways. For example:
- screening helps to keep people who may be infectious out of the workplace
- good ventilation and wearing masks can help reduce the amount of virus in an indoor space
- maintaining physical distance reduces the chance of being exposed to respiratory droplets of all sizes
- personal protective equipment(PPE) can help protect the wearer from exposure to the virus and may be required when other control measures cannot be consistently maintained
The best way to reduce the likelihood of transmission in your workplace is to have multiple controls in place. This is especially important in situations where one or more controls cannot be consistently maintained.
COVID‑19 vaccines may supplement, but should not replace, any workplace controls. No single action, including vaccination, is perfect at controlling risks. Workplace control measures reduce the chance of people being exposed to the virus. Vaccination reduces the chance that the person vaccinated will get sick if they are exposed to COVID‑19.
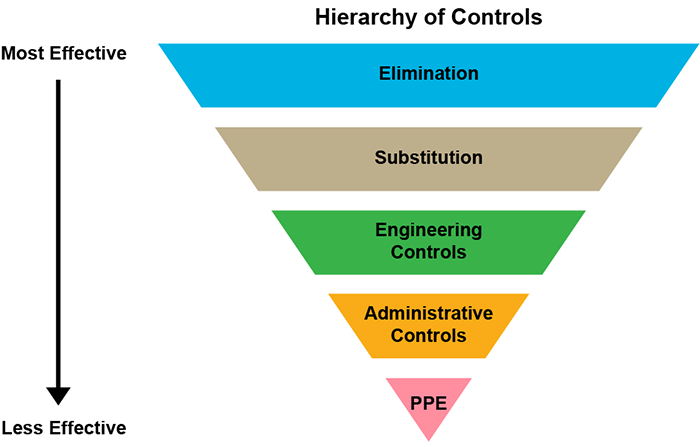
Use the hierarchy of controls
The hierarchy of controls (image and description below) can help you choose the right controls for your workplace. This applies to all workplace hazards, not just COVID‑19 .
The levels in the hierarchy of controls, in order from most effective to least effective, are:
- elimination
- substitution
- engineering controls
- administrative controls
- personal protective equipment (PPE)
When making your plan, always start by considering the most effective controls first. First, try to eliminate the hazard altogether. Where eliminating the hazard is not possible, use multiple engineering and administrative controls.
The higher the control appears in the diagram and the earlier it is in the list, the more effective it is. The first three types of controls are more effective because once in place they do not usually require additional action by a worker. The effective use of administrative controls and PPE requires workers and other people to implement them properly and consistently every time.
Even with the rapid and collaborative response to COVID‑19 , there are still many uncertainties about the disease. As the evidence evolves, what we know about the risks and best practices for controls may change, so it is important to stay current. The safety plan approach allows you to incorporate new information as it becomes available.
Elimination
Remove the risk of exposure entirely from the workplace. For example, having everyone work from home all the time would eliminate COVID‑19 risk from a workplace.
Substitution
Replace a hazardous substance with something less hazardous (for example, replace one chemical with another). For an infectious disease such as COVID‑19 , substitution is not an option.
Engineering controls
Make physical changes to reduce or remove the hazard, for example, through ventilation or separating workers from the hazard.
Administrative controls
Make changes to the ways people work and interact, using policies, procedures, training and signage. For example, you could:
- establish contactless curbside pickup
- create policies to limit the number of people in a space at one time
- schedule to stagger work shifts and breaks
- establish new cleaning and disinfection protocols
- provide education and training on proper hand washing technique
- set up a screening process
Personal protective equipment (PPE)
This is equipment and clothing worn by a worker to minimize exposure to hazards and prevent illnesses and infection. PPE is used to protect the wearer and can include such things as surgical/procedure masks and eye protection.
Correct use of PPE can help prevent some exposures, but it should not take the place of other control measures, for example, screening, hand hygiene, use of barriers and physical distancing where possible. PPE must be used alongside other control measures already in place.
Using masks as a control measure
A mask is a piece of equipment that covers the wearer’s nose, mouth and chin. It is fixed to the face with straps, ties or elastic, either behind the head or with ear loops.
For COVID‑19 protection, masks can be used as workplace control measures in two ways:
- as source control: workers and visitors wear the mask to protect those around them
- as personal protective equipment (PPE): workers wear the mask (along with eye protection) to protect themselves
Not all masks are suitable for both purposes, however, many masks that are suitable for use as PPE also work for source control. You need to consider how you will use the mask in your workplace and make sure to select a suitable type of mask. Cloth masks are not PPE.
How effective masks are as a control measure depends on:
- the type of mask(s) used
- masks being worn properly and consistently
It is recommended that all workers wear masks that provide source control:
- indoors at all times
- outdoors where physical distance cannot be maintained
To help you decide what is right for your workplace, see using masks in the workplace for more information.
Safety plan questions
There are six questions you should think through as you develop your COVID‑19 workplace safety plan. The information in this document will help you to think through the issues as you develop a plan for the unique situation in your workplace.
Question 1: How will you ensure all workers know how to keep themselves safe from exposure to COVID‑19 ?
Provide clear information and instruction to your workers. Make sure they know what they need to do to protect themselves and others. Ensure they know how to follow the work and hygiene practices in your plan, including all new safety measures.
Set up or use your current internal communication systems to provide frequent reminders and updates. Use a variety of ways to reach your workers, such as:
- posting notices in common areas
- emails
- virtual team meetings
- intercom announcements
Keep up with public health and workplace safety guidance for COVID‑19 . Share new information as soon as possible.
Some actions to consider:
- post information for workers and other people entering the workplace
- share information in all languages spoken by your workers, if possible
- use easy-to-understand information, such as graphics and resources from the Ontario government
- provide information to your workers about how vaccination can help keep them safe
- remind workers about available social and mental health supports, and encourage them to use these resources
- share information to help your workers stay healthy while commuting and travelling as part of their work
- train and re-train on procedures
Question 2: How will you screen for COVID‑19 ?
Screening helps keep infected workers and others from entering the workplace. This can reduce possible transmission in your workplace. Read more about workplace screening .
Make sure all workers know to stay home if they have symptoms that are new, getting worse or unexplained (for example, not caused by an existing condition). Provide information to workers on how to access health, job and financial supports that are available to them.
Know the symptoms and risk factors to look for and plan for how you will screen workers and others who enter your workplace. You must make sure that your screening process follows the instructions issued by the Office of the Chief Medical Officer of Health.
Make sure any people working as screeners receive information and instruction on how to perform this work safely and what to do if a person must be excluded from the workplace.
Screening of workers
Employers must actively screen all workers, including those who are vaccinated, for COVID-19 symptoms and other risk factors before they enter the workplace at the start of their shift.
Active screening means that as an employer it is your responsibility to ensure that no worker enters the workplace unless it is confirmed they have completed the screening and the result of that screening has indicated that they are allowed to enter the workplace.
Consider what records you will keep so you can show how your active screening process works and that you have been following it.
Question-based screening
This type of screening involves using information about symptoms and exposures to determine if a person can enter a workplace.
A person has passed question-based screening if they have none of the symptoms or exposures asked about in the screening tool.
You can use the COVID-19 worker and employee screening tool or must make sure your screening tool includes all the same questions.
Question-based screening may be done in person or remotely, including by telephone, web tool, email or app.
Rapid antigen screening
This screening method involves collection of a sample from an individual that is analysed to see if it contains proteins from the SARS-CoV-2 virus. Rapid antigen screening is used to help identify asymptomatic COVID-19 cases.
A person has passed rapid antigen screening if they get a negative result on the rapid antigen test. Individuals with a positive result obtained through a rapid antigen screening do not require a PCR test to confirm the result.
Rapid antigen screening can be a helpful step to add to a workplace screening process. If you are thinking of adding rapid antigen screening in your workplace, read more about considerations and get free rapid tests.
Self-monitoring
Encourage workers to monitor their own symptoms at all times, including while at work:
- ensure workers know what to do if they start to experience symptoms at work
- let workers know where to find the online COVID-19 self-assessment tool
- ask workers to use the self-assessment tool at home if they have any symptoms and to follow the instructions
Make sure workers know who their workplace contact is and how to get in touch with them in case the self-assessment, public health or their health care provider tells the worker to self-isolate.
Screening of non-workers
Consider how you will screen clients, customers and patrons. Where possible, actively screen using the COVID-19 customer screening tool. Note that in some workplaces, there may be requirements for active screening of non-workers. Proof of vaccination may be required as part of the screening process for non-worker in some settings.
You may be able to screen non-workers:
- by phone or online before they arrive
- using a process similar to the one that you use to screen your workers
At a minimum, you must have passive screening of non-workers entering your workplace. This means:
- you must post signs with clear instructions at all entrances that tell people how to screen themselves
- the signs should include the screening questions and instruct people with symptoms or high-risk exposures not to enter the premises
- people are assumed to have screened themselves and followed the instructions
- you do not need to ask anyone to report the result of their screening
- a person should be told not to enter if they volunteer the information that they did not pass the screening assessment
Screening results – next steps
If a person, worker or non-worker, passes all steps used in the screening they:
- are permitted to enter the workplace at that time
- must continue to follow all public health and workplace control measures, including masking, maintaining physical distance and hand hygiene
- should continue to self-monitor and workers should follow their workplace’s reporting procedure if they develop symptoms during their shift
If a person, worker or non-worker, does not pass on any part of the screening they:
- are NOT permitted to enter the workplace at that time
- must follow guidance on self-isolation and return to work.
Question 3: How will you control the risk of transmission in your workplace?
COVID‑19 can be spread by people who do not have symptoms even after being vaccinated. This is why it is very important to have effective control measures in the workplace.
Examples of controls to consider are provided below. You can find many other ideas in the sector-specific resources to prevent COVID‑19 in the workplace.
To operate your business more safely and to keep it operating, you may need to make changes to the workspace and to the ways your work is done.
Maximize physical distancing and separation
The most effective way to reduce the risk of COVID‑19 transmission is to avoid in-person interactions. Where possible, workers should continue to work from home and meet virtually until public health authorities advise otherwise.
Where remote work is not possible, maintaining physical distance is an important measure to reduce the chance of transmission. To enable workers to maintain a physical distance of at least two metres from other people in the workplace, use a variety of engineering and administrative controls, such as:
- barriers, such as plexiglass, to maintain separation as a primary means of control
- scheduling and other administrative changes to reduce the number of people who must share the same space including during shifts, lunch and other breaks
- providing adequate space by using and repurposing all available areas inside your facility and in the surrounding outdoor space
Source control masking
Using masks as source control involves having workers, visitors and clients in the workplace wear a mask to help protect those around them. All employers should use source control masking, combined with other control measures. Masks are especially important indoors and help to reduce the risk in situations where:
- workers spend time together or one after another in an enclosed or confined area
- there is poor ventilation
- a lot of people are in the same space
- physical distancing cannot be consistently maintained
Source control masks should not be used instead of physical distancing, and physical distancing should not be used instead of source control masks – both control measures lower risk and should be used together.
Consider how effective using masks as source control may be in your workplace. This will depend on the type of mask(s) used and whether they are worn properly and consistently.
Encourage clients, customers and visitors to your workplace to wear masks to help protect your workers and to reduce the risk of transmission of COVID‑19 in your community.
In some workplaces in Ontario, wearing a mask or face covering is required by public health or other authorities. You should be aware of the most current:
- requirements of the local public health unit
- relevant bylaws in the municipality in which you do business
- requirements under the Reopening Ontario (A Flexible Response to COVID‑19 ) Act that are applicable to your business
- directives issued by the Chief Medical Officer of Health that are applicable to your industry or business
Even with other controls in place including physical distancing and source control masking, there may be situations where PPE will be required. A surgical or procedure mask worn as part of required PPE also works as source control. Masks, including respirators, with exhalation valves should not be used for source control.
Ventilation and air flow
The risk of COVID‑19 transmission is higher in more enclosed and crowded spaces. Good ventilation can decrease the concentration of aerosols that may be suspended in the air indoors and help reduce the chance of COVID‑19 spread.
Ventilation includes:
- dilution – opening windows and doors, increasing air exchange rates in air handling (HVAC) systems
- filtration – using filters to remove viral particles from the air
At minimum, you should ensure that HVAC systems are maintained according to the manufacturer’s instructions. Consider COVID‑19 standards for ventilation and HVAC systems, such as those from the CSA Group and the ASHRAE.
Additional steps you can take:
- use portable air cleaners
- keep windows and doors open as much as possible, including in colder weather
- adjust HVAC systems to increase the amount of fresh air and reduce recirculation
- continue ventilation and air exchange after regular business hours
- run exhaust fans at full capacity (for example in bathrooms and kitchens)
- if fans are needed for temperature control, make sure you are using them as safely as possible
- use available outdoor space whenever possible (for example, for meetings, breaks, client interactions such as curbside pick-up)
- consider going beyond minimum standards if possible
- carbon dioxide (CO2) sensors may be used to help identify areas with poor ventilation
- they cannot identify the presence or absence of COVID‑19 in the air
Ventilation improvements should not be used instead of other control measures, such as source control masking and other controls should not be used instead of ventilation – all control measures lower risk and should be used together. The use of other control measures is particularly important in areas where it is difficult to improve ventilation.
Reduce transmission from surfaces and objects
The virus that causes COVID‑19 may be transferred to surfaces or objects. Workers can be infected if they touch their face with contaminated hands.
Consider the policies and procedures you can put in place to make sure you are cleaning and disinfecting and keeping the workplace as free of the virus as possible. The public health recommendation is to clean and disinfect high-touch surfaces at least twice a day.
To reduce transmission:
- identify commonly touched surfaces and commonly used areas in your workplace and put into place a schedule to clean and disinfect them
- consider whether there are high-touch surfaces that may need to be cleaned and disinfected more often
- assign tools, equipment and workstations to a single user if possible, or limit the number of users
- regularly clean and disinfect any shared equipment and tools, including between users
Support good hand and respiratory hygiene
The same everyday steps recommended by public health officials to stop the spread of COVID‑19 are important in the workplace too. One of the most important things we can all do is to wash our hands often with soap and water.
Think about what you can do to make it easier for your workers to take these steps regularly at work. You can:
- post reminders to wash hands, use proper cough and sneeze etiquette and avoid touching eyes, nose or mouth
- provide ways to properly clean hands by providing access to soap and water and, if that is not possible, alcohol-based hand sanitizer
- ensure that workers can clean their hands frequently and whenever needed
- have all workers and visitors properly clean their hands before entering the workplace and after contact with objects and surfaces others may have touched
Personal protective equipment
To determine when personal protective equipment (PPE) is needed in your workplace, you will need to assess all the relevant factors in the workplace. This includes how effective the other control measures you have in place are. Even with other controls in place there are situations where PPE will be needed.
Correct use of PPE can help prevent some exposures, but it should not take the place of other control measures – PPE must be used alongside other control measures already in place.
It’s important that any PPE workers use is appropriate for the purpose. The effectiveness of PPE depends on every person wearing it correctly and consistently. Make sure your workers are trained on the care, use and limitations of any PPE that they use.
The Chief Medical Officer of Health has provided direction to health care organizations about the minimum requirements for COVID‑19 PPE.
Where PPE for COVID‑19 is needed in non-health care settings:
- it will likely consist of a surgical or procedure mask (or equal or greater protection) in addition to eye protection (such as face shield or goggles)
- gloves will not usually be needed as they do not provide any more protection than hand washing or using hand sanitizer
Workers that wear PPE for protection against workplace hazards besides COVID‑19 must continue to use that PPE as required. This includes gloves for new cleaning and disinfecting products that workers use because of COVID‑19 .
Question 4: What will you do if there is a potential case of, or suspected exposure to, COVID‑19 at your workplace?
There are steps that you will need to take if one of your workers, visitors or clients has symptoms that may be related to COVID‑19 or is diagnosed with COVID‑19 :
Step 1: Exclude people with symptoms or who have been exposed from the workplace
Workers should be kept out of the workplace if any of the following are true:
- they have they have tested positive for COVID‑19
- they have been exposed to someone with or who has received a positive test result (details may vary based on vaccination status and type of exposure – see for more information)
Special requirements apply to people who live, work, attend or volunteer in high-risk settings, such as health care settings, congregate living settings, and First Nations, Inuit, and Métis communities.
Clients and customers who have COVID‑19 symptoms or some types of exposures should be screened out of the workplace based on the directions in the screening guidance.
If a worker calls in sick, informs you of symptoms of COVID‑19 or informs you they had close contact with someone with symptoms, have them take the self-assessment. Ask the worker to follow any recommendations given by the tool, including being tested and self-isolating.
If anyone shows symptoms in the workplace, they should return home and self-isolate immediately. If they cannot leave immediately, they should be isolated until they are able to leave. Have a plan in place to deal with this and train supervisors on how to handle the situation.
Self-isolation and return-to-work
A person who has COVID‑19 must self-isolate so they can’t infect others, whether fully vaccinated or not. The purpose of self-isolation after exposure is to prevent a person from infecting others before they know they are infected.
As an employer, it is important for you to understand COVID‑19 self-isolation and return to work for your workplace. Details on requirements can be found in the provincial guidance on the management of cases and contacts of COVID‑19. Follow any and all public health measures and direction.
Consider how you can support workers so they are able to self-isolate and how you will manage if workers are unavailable. You could:
- assign work-at-home tasks to workers who must
- use flexible schedules that allow self-isolating workers to work additional hours when they return to the workplace
- identify workers within your organization who can work additional hours or shifts as needed and make sure they are trained to do the work they might be asked to do
- develop back-up schedules that can be quickly implemented if needed
- make sure workers know how to access job and financial supports that are available to them and provide them any documentation they need
Workers who are considered employees under the Employment Standards Act have the right to take job-protected infectious disease emergency leave if they must self-isolate because of COVID‑19.
You cannot penalize an employee in any way for taking or planning on taking an infectious disease emergency leave.
Learn about the Ontario COVID‑19 worker income protection benefit.
Workers who must take time off from work because of COVID‑19 may be entitled to employment insurance benefits or to other federal government financial supports. For information, visit the federal government’s website or contact Service Canada’s Employment Insurance Automated Telephone Information Service at
Workers can return to the workplace after their self-isolation period if they have no fever and their symptoms have been improving for the appropriate time period, based on the appropriate time period, based on the guidance provided by the Ministry of Health.
Workers do not need a negative COVID‑19 test to return to the workplace after self-isolating for the full required period.
Step 2: Inform any workers who may have been exposed
Let workers know if they may have been exposed in the workplace.
If available, provide information to workers about the potential exposure and where it took place. Don’t give out information that will identify the infectious person.
Having a system in place to help keep track of which people had can help you identify who may have been exposed if someone in your workplace develops symptoms or tests positive for COVID‑19.
You could include information such as:
- dates and times of interactions
- approximate length and frequency of interactions
- full names
- contact telephone numbers
- addresses (for workers) or the name of the visitor’s business
Some businesses may be required to collect and maintain contact information. Information on minimum requirements can be found in the Reopening Ontario (A Flexible Response to COVID‑19) Act.
In places where active screening of patrons is not required, businesses should and ask all clients and customers to for COVID‑19 symptoms or exposures prior to entry to the workplace.
Step 3: Report to Ministry of Labour, Training and Skills Development and the WSIB
If you are advised that one of your workers has COVID‑19 due to exposure at the workplace, or that a claim has been filed with the Workplace Safety and Insurance Board (WSIB), you must give notice in writing within four days to:
- the Ministry of Labour, Training and Skills Development
- the workplace’s joint health and safety committee or health and safety representative
- the worker’s trade union (if applicable)
Additionally, you must report any occupationally acquired illnesses to the WSIB within three days of receiving notification of the illness.
You do not need to determine where a case was acquired and you do not need proof of a positive COVID‑19 test. If it’s reported to you as an occupational illness, you must report the case.
Question 5: How will you manage any new risks caused by changes to the way you operate your business?
Changes to work practices to prevent COVID‑19 may affect the way you manage other risks in the workplace. For example, you may have controlled the risk of injury from lifting heavy items by having two people involved. This may not be possible while workers maintain physical distance.
It’s also possible that new procedures will bring new risks or challenges. For example, if you start using a new product for disinfection, you need to know what chemicals are in the product and how to use it safely. Workers may need new training.
Other plans and protocols you have in place may also need to be adapted for COVID‑19 . For example, how will you maintain physical distance during an emergency evacuation? What will you do if workers are told to self-isolate because of exposure to COVID‑19?
Review and update your workplace violence prevention policy to address the potential for increased risks of harassment, threats and violence to workers. Have a clear process for dealing with aggressive or violent behaviours, particularly when workers are conducting screening, requiring proof of vaccination or are asked to inform customers about COVID‑19 protocols. Make sure these workers get the information and instruction they need to do their work as safely as possible.
Remote work may pose its own risks. This may include technological barriers, mental health concerns and ergonomic challenges.
New risks may be introduced by:
- workers having been away from their work
- changes to processes and procedures
- use of temporary labour and inexperienced staff
- restarting activities and machinery that have been shut down
- stress and change – consider how this affects your workers’ mental health
If your plan introduces shift work or splits teams that would normally work together, describe what steps you’ll take to:
- manage the impacts of shift work, including fatigue, transport, childcare and the potential dilution of skills available within a split team or rostered workgroup
- ensure each team has access to the right skills and support to be able to work safely
Question 6: How will you make sure your plan is working?
Operating a business during the pandemic involves recovery stages will involve different ways of working. Checking to see how your plan is working will help you find the best solutions for your unique situation and adapt to any changes.
You may want to assign a manager or management team to take charge of COVID-related issues, including training for supervisors and regular dialogue with supervisors, to make sure there is compliance with all protocols. Use existing incident reporting systems. Schedule regular times to review your plan and its effectiveness.
Consider:
- How will your health and safety representatives or JHSC be involved in evaluating how well the plan is working?
- Add your COVID‑19 measures and procedures to the JHSC checklist for required monthly inspections.
- In health care workplaces the joint health and safety committee or health and safety representatives must be consulted.
- What is the best way to engage your workers and workplace parties? Ask them how they would like to participate in decision making and provide feedback. Remember it may not be possible for them to complete forms or attend meetings outside of work time.
- What can you measure and monitor so that you can evaluate how well the new protocols are being followed?
- How will you communicate changes to processes, ensure all workers know about the changes and are trained to implement them?
- How often will you update and share new versions of your plan?
As the COVID‑19 situation evolves what is right for your situation may change. Make sure to review and update your plan regularly.