Recognize and temporarily reverse an opioid overdose
Naloxone can temporarily reverse an opioid overdose. Learn how to recognize an opioid overdose and use naloxone to reverse it.
Free naloxone kits for individuals
If you are with someone who has overdosed, call 911 immediately.
Don’t let legal fears stop you from getting help. Federal laws provide some legal protection if you experience or witness an overdose and call 911 for help.
What naloxone does
Naloxone (pronounced na-LOX-own,) is a drug that can temporarily reverse and opioid overdose. Opioids are drugs that can be used to treat pain, and some people use opioids to get high. Some commonly used opioids include:
- hydromorphone
- fentanyl or carfentanil
- morphine
- heroin
- methadone
- oxycodone
When someone overdoses on opioids, their breathing either slows or stops completely. If used right away, naloxone can help them breathe again. Naloxone can either be injected or given as a nasal spray.
Who can get a free naloxone kit
You are eligible for a free naloxone kit if you are:
- at risk of an opioid overdose
- an individual’s friends, family, or other individuals in a position to assist the individual at-risk
- a client of a needle exchange program, hepatitis C program or consumption and treatment service
- being released from a correctional facility
Where to get a free naloxone kit
Search our map of pharmacies and community organizations that shows where you can get naloxone kits and training on how to use them.
Pharmacies
Not all pharmacies carry naloxone kits. Call ahead to check if your pharmacy has naloxone kits in stock. You can also ask the pharmacist any questions you might have.
Participating Ontario pharmacies offer free injectable and nasal spray naloxone kits. You do not need a prescription or an Ontario health card to get a naloxone kit. The pharmacist will train you on how to recognize an opioid overdose and explain how to use the naloxone kit.
Community-based organizations
Please note: Only individuals at risk of opioid overdose and their friends and family can access naloxone kits from community-based organizations.
You do not need a prescription or an Ontario health card to get free injectable kits or nasal spray naloxone kits from participating:
- needle syringe programs
- hepatitis C programs
- public health units
- Aboriginal Health Access Centres
- AIDS service organizations
- Community Health Centres
- outreach programs
- withdrawal management programs
- shelters
- hospitals with an emergency department or urgent care centre
The program staff will train you on how to recognize an opioid overdose and how to use the injectable or nasal spray naloxone kit.
Provincial correctional facilities
Inmates from provincial correctional facilities are eligible to be trained on how to use nasal spray naloxone and provided kits when they are released from custody.
What is in a naloxone kit
Injectable kits
Each injectable naloxone kit includes:
- 1 hard case (for example, a zippered hard black case with red “naloxone” cross)
- 2 (0.4 mg/1 mL) vials or ampoules (a small glass container) of naloxone
- 2 safety-engineered syringes with 25G, 1” needles attached
- 2 alcohol swabs
- 2 devices (known as “breakers,” “snappers,” or “openers”) for opening ampoules safely
- 1 rescue breathing barrier
- 1 pair of non-latex gloves
- 1 card that identifies the person who is trained to give the naloxone
- 1 insert with instructions (English and French)

Nasal spray kits
Each nasal spray naloxone kit includes:
- 1 hard case (for example, a zippered hard black case with red “naloxone” cross)
- 2 doses of naloxone hydrochloride intra-nasal spray (4 mg/0.1mL)
- 1 rescue breathing barrier
- 1 pair of non-latex gloves
- 1 card that identifies the person who is trained to give the naloxone
- 1 insert with instructions (English and French)
Check the expiry date
Naloxone has an expiry date. The expiry date is written on the ampoules or vials (for injectable naloxone) or on the nasal spray device.
If you have expired naloxone, get a new kit. You should return any unused or expired naloxone kits to your nearest pharmacy.
How to recognize an opioid overdose
Don’t let legal fears stop you from getting help. Federal laws provide some legal protection if you experience or witness an overdose and call 911 for help.
Someone may have overdosed if they:
- can’t stay awake, walk or talk clearly
- are breathing slowly or not at all
- have a limp body or muscles are rigid
Other signs of overdose include:
- not responding to noise or shaking of shoulders
- snoring or gurgling sounds
- pale or blue, grey or purple skin — especially on their nail beds and lips — and they feel cold
- tiny pupils (pinpoint) or their eyes are rolled back
- vomiting
How to use a naloxone kit
When you receive a naloxone kit, you will be trained on how to use it.
If you are with someone who is having an opioid overdose:
- shout their name and shake their shoulders
- call 9-1-1 if they are unresponsive
- give naloxone:
- (if using an injectable kit): inject 1 vial or ampoule (a small glass container) (0.4 mg/1 mL) of naloxone into their arm or leg
- (if using a nasal spray kit): lay the person on their back, insert the tip of nozzle into one nostril and press the plunger firmly
- rescue breathing and/or chest compressions
- if there is no improvement after 2-3 minutes, repeat steps 3 and 4. Stay with them.
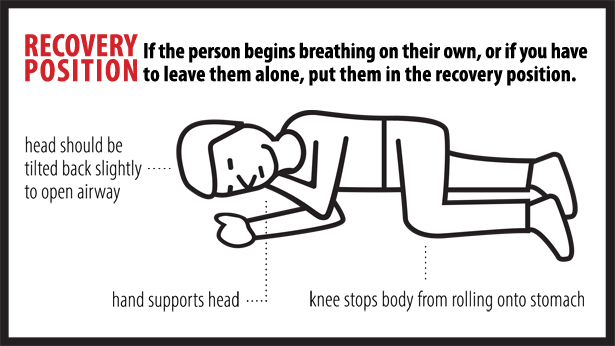
If the person begins breathing on their own, or if you have to leave them on their own, put them in the recovery position.
Stay until the ambulance arrives in case paramedics need help or information, or the overdose symptoms return. With more powerful opioids (fentanyl and carfentanil) there is a possibility that a person will overdose again even after they have been given naloxone and even if they don’t use more drugs.
Note: This information is intended to reduce the harms related to drug use, including deaths.

